Do you often experience digestive stress after eating certain foods?
Can the discomfort be so severe that it affects your day-to-day activities?
The link between foods and digestive disorders is well recognised, and there is a good chance that FODMAPs – small carbohydrates in certain foods – may be the culprit.
As a food intolerance dietitian, I’ve seen how remarkable a low-FODMAP diet can be for people with chronic gastrointestinal symptoms… things like recurrent bloating, gas, cramps, diarrhea or constipation. This diet is one of the natural ways known to alleviate such chronic symptoms.
There’s also many new case studies suggesting it can help manage symptoms of other health issues too.
If you’re keen to learn more, and maybe even try a low FODMAP diet for yourself, this 3,000 word beginner’s guide is a great place to start.
Note that each section in this article has a ‘summary’ box (like this one) to save time. Below this box is a contents menu to help you navigate directly to a particular section.
What Are FODMAPs?

A low FODMAP diet is also known as a FODMAP elimination diet.
This is a temporary eating pattern that has a very low amount of food compounds called FODMAPs.
The acronym stands for:
- Fermentable – meaning they are broken down (fermented) by bacteria in the large bowel
- Oligosaccharides – “oligo” means “few” and “saccharide” means sugar. These molecules are made up of individual sugars joined together in a chain
- Disaccharides – “di” means two. This is a double sugar molecule
- Monosaccharides – “mono” means single. This is a single sugar molecule
- And Polyols – these are sugar alcohols (however, they don’t lead to intoxication!)
As you can see, there are four main saccharide groups that make up FODMAPs – oligosaccharides, disaccharides, monosaccharides and polyols.
These FODMAP groups have specific names and may also have more than one group within them, known as a FODMAP subgroup:
- Oligosaccharides have two subgroups, known as fructans and galactans (or galacto-oligosaccharides or GOS for short)
- Disaccharides are known as lactose and only contain one group
- Monosaccharides are known as fructose (or excess fructose) and also only contain one group
- Polyols have two subgroups, known as sorbitol and mannitol
Let’s stick with the term FODMAPs shall we?
Those saccharides and polyols are short-chain carbohydrates that, if poorly digested, ferment in the lower part of your large intestine (bowel).
This fermentation process draws in water and produces carbon dioxide, hydrogen, and/or methane gas that causes the intestine to stretch and expand.
The result is strong pain, bloating, visible abdominal distension and other related symptoms (1).
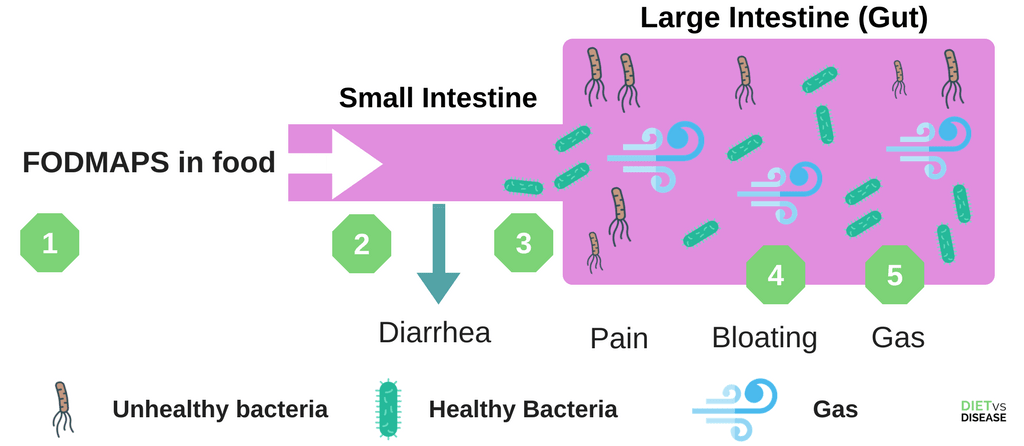
- Food is eaten that contains FODMAPs.
- Some FODMAPs may pull water into the small intestine, causing diarrhea
- In those with IBS, FODMAPs can travel to the large intestine (gut) largely undigested.
- When “unhealthy” bacteria interact with FODMAPs in the gut, it causes a range of symptoms such as bloating, gas and pain.
- Different people are sensitive to different FODMAPs, so it’s important to identify which ones are the culprit.
This is a video training I made that explains FODMAPs and the low FODMAP diet if you prefer to watch instead of read:
What is a low FODMAP diet?
The primary use of this diet is to relieve digestion-related symptoms, but is emerging as a useful tool for several other conditions too.
It can be useful for those with:
- Irritable Bowel Syndrome (IBS)- more on that below
- Other forms of Functional Gastrointestinal Disorder (FGID)
- Small intestinal bacterial overgrowth (SIBO)
- Certain auto-immune conditions/diseases like (potentially) rheumatoid arthritis, multiple sclerosis or eczema
- Fibromyalgia or other health issues you’ve noticed are triggered by certain foods
- Frequent migraines that appear to be triggered after certain meals
- Inflammatory bowel disease (IBD) such as Crohn’s disease, ulcerative and microscopic colitis.
The best candidates for trialling this diet also tend to answer yes to these questions.
And note that it’s not to be confused with a food chemical intolerance such as a low Histamine Diet or a low Salicylate diet.
Summary: FODMAPS are short-chain carbohydrates that, if poorly digested, ferment in the bowel to cause severe digestive stress. This diet is designed to temporarily restrict the amount of FODMAPs consumed and is useful for treating conditions like IBS.
The “What Can I Eat on a FODMAP Diet?” food list
This is a giant list of what foods to eat, and what foods to avoid when following a low FODMAP diet.
It’s based on the latest published FODMAPs data (7, 8, 9, 10, 11).
It looks like this:
You can download a large and printable 4-page PDF version now by tapping the blue button below:
Many legumes not included on this list (such as chickpeas and lentils) can be made far more digestible and low FODMAP by pre-soaking for 7-24 hours.
Also note that like with anything food related, portion size is fundamental. A serving of 10 almonds are considered low FODMAP, but if you eat 20 almonds then you will end up eating a high amount of FODMAPs.
As with anything we eat, the dose makes the poison.
Summary: Above is a list of high and low FODMAP foods that you can take with you when grocery shopping. Remember that many of these foods still contain trace amounts, so portion size is fundamental.
Common FODMAPS and what to look for on the label

Common FODMAPs in your food include:
- Fructose: A sugar found in most fruits and vegetables.
- Lactose: A sugar found in dairy foods like milk.
- Fructans: A chain of sugars found in many vegetables and grains.
- Galactans: Found primarily in legumes.
- Polyols: Sugar alcohols like sorbitol and mannitol. You find them mainly in artificial sweeteners and chewing gum but they are also naturally occurring in various fruits and vegetables.
The Monash University low FODMAP diet phone app is a great place to start when reading food labels.
You can check the app for foods that have been tested as high FODMAP.
It’s also useful to know other common high FODMAP ingredients such as inulin (chicory root), natural flavors, high fructose corn syrup, agave, honey, etc so you can avoid them also.
Is Gluten a FODMAP?
While gluten can also trigger food sensitivities in a handful of people, it is a protein, not a carbohydrate.
Therefore gluten cannot be classified as a FODMAP.
However, gluten-free products do still appear beneficial for those with FODMAP sensitivities. Testing from Australia’s Monash University shows that gluten-free products almost always have reduced amounts of fructans and oligosaccharides.
This is because gluten and FODMAPs often co-exist in the same product e.g. wheat bread and pasta.
So by choosing gluten-free products means that they are also more likely to be lower in FODMAPs, and free of gluten of course.
Summary: FODMAPs exist mainly in dairy, legumes, and many fruits and vegetables. While gluten is not technically a FODMAP, gluten-free products are typically lower in FODMAPs anyway.
A low FODMAP diet is very restrictive and designed to be temporary

Before we go any further, it’s important to clarify that following a low FODMAP diet is very restrictive and cuts out numerous common foods and food groups.
That means you need to reintroduce foods at some stage, so it cannot be a permanent solution.
The idea is that restricting all FODMAPs at once should have a far greater and more consistent effect than simply restricting one FODMAP in isolation. By reducing all high FODMAP foods, your intake of FODMAPs will reduce to a level where you no longer get symptoms.
How it works
There are three phases of the low FODMAP diet.
- Phase 1 – Elimination/Strict low FODMAP Diet: For 3-8 weeks (depends on how you respond) you strictly exclude all high FODMAP foods from your diet.
- Phase 2 – Reintroduction/Rechallenge: You will reintroduce each FODMAP group one at a time to see what triggers symptoms. For example, you may first reintroduce fructose for three days. If you have no symptoms, you may then reintroduce lactose too, and so on.
- Phase 3 – Modified/Adapted FODMAP Diet: Once the trigger FODMAPs have been identified, you will know what you can and cannot eat. You can then use this information to formulate your own personalised diet that keeps your symptoms to a minimum.
Summary: This diet is not designed to be permanent. It is highly restrictive for several weeks, before foods are slowly reintroduced to determine what causes symptoms.
IBS and studies that support a low FODMAP diet

Much of the research has been on patients with Irritable Bowel Syndrome (IBS).
IBS is a chronic gastrointestinal disorder characterised by abdominal pain and altered bowel habits, and around two thirds of IBS patients report their symptoms are related to food.
It’s now estimated to affect 11% of the population globally, up to 13% in Australia and up to a whopping 20% in the US and UK (2, 3).
One landmark clinical trial compared the responses of 39 IBS patients who received standard healthy eating advice against 43 IBS patients who received low FODMAP training from a dietitian (13).
Can you guess what diet is best for IBS?
I’ve illustrated some of the results here below in this chart. The black bar represents those in the standard diet advice group, the pink bars are those in the low FODMAP group.
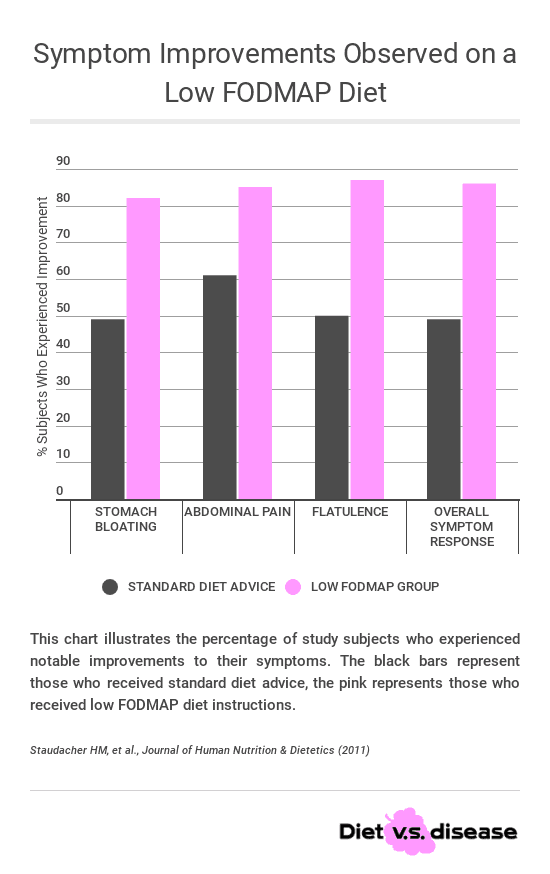
While diet changes helped for both groups (as expected), the number of subjects who experienced an improvement in IBS symptoms was far greater in the low FODMAP group compared to the standard group.
Basically almost 9 out of every 10 people on the FODMAP diet had huge improvements in bloating, stomach pain, flatulence and their overall symptoms.
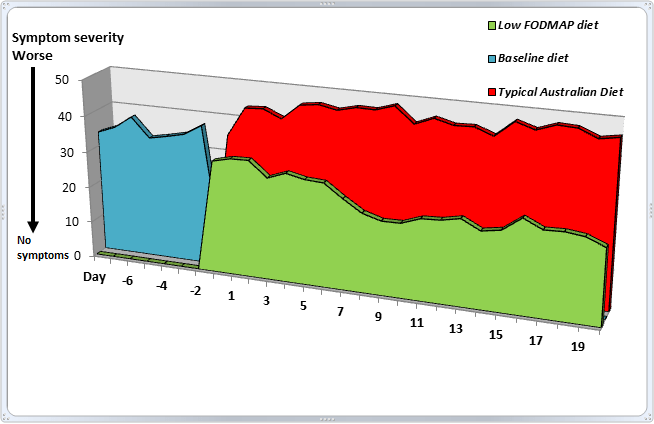
Another high quality study was an Australian clinical trial that compared the effects of a low FODMAP diet between 30 IBS patients and 8 similar individuals without IBS (to act as a control group for comparison) (4).
Participants were randomly assigned to receive either a diet low in FODMAPs (less than 3 grams per day) or a typical Australian diet for 21 days. This was followed by a long “washout period”, before crossing over to the alternate diet for another 21 days. Almost all food was provided to the participants, and breath hydrogen and stool samples were collected frequently.
This is what happened:
Click to enlarge.
IBS symptoms were reduced by 50% overall on the low FODMAP diet, with the greatest improvements observed one week after implementing the diet. More specifically, improvements were seen for bloating, abdominal pain, wind and dissatisfaction with stool consistency.
Numerous similar studies (albeit not as well designed) have found very similar benefits, and the overall average success rate is about 68-76% of patients (5, 6).
Research in this area still has a way to go, but many doctors now recommend it as the first dietary approach for treatment of recurrent gastrointestinal issues.
Summary: Controlled trials continue to find that a well-designed and supervised low FODMAP diet improves symptoms by about 50% in as little as one week. The average success rate is 68-75% of patients that try it, based on the studies mentioned above.
Low FODMAP recipe ideas
Appropriate recipes are those low in total FODMAPs, yet still nutritious and simple to make (and delicious of course).
To save you time searching around all day, I’ve compiled a roundup of low FODMAP recipes for mains and snacks that are not only family-friendly, but easy to bring to work too:
- 25 Scrumptious Low FODMAP Breakfast Recipes To Start Your Day
- 25 Tasty Low FODMAP Lunch Recipes For IBS
- 30 Delicious Low FODMAP Dinner Recipes: Don’t Get Stuck Eating The Same Thing!
- 77 Easy and Tasty Low FODMAP Snacks: You Don’t Have To Miss Out
- 30 Delicious Low FODMAP Vegetarian And Vegan Recipes Plus Some FAQ
Probiotics may help ease symptoms but it’s unclear

Recent data suggests there is a strong link between the balance of our gut bacteria (called the gut microbiota) and health.
An imbalance of this bacterial “community” – known medically as gut dysbiosis – can cause many problems… especially gut issues.
Probiotics is the term used to describe the bacteria we eat specifically for to restore this balance and improve health.
So how does this relate to FODMAPs?
Growing evidence shows that many subgroups of IBS patients have a highly irregular gut bacterial environment (7).
The question posed now is will the addition of “good” bacteria – from probiotics – help to manage FODMAP sensitivities? The research is promising, and I’ve written a detailed review and guide here.
Essentially from that review it appears that the probiotic supplements VSL#3, Symprove and Align/Alflorex are the most useful. If you are predominantly dealing with occasional irregularity then look for a probiotic with a mixture of Lactobacilli species.
Whole food sources of probiotics include fermented foods like quark, kefir yoghurt and pickled vegetables such as sauerkraut. Apart from the fact that many of these probiotic containing foods are high FODMAP and so are not well tolerated by many, there are several potential problems relying on whole foods for probiotics.
For example, each batch of food will vary in their active probiotic strains and concentration. Additionally, fermented foods are rich in food chemicals like salicylates and histamine, which some people may also be sensitive to (9).
This fact should be considered on an individual basis.
Summary: Poorly absorbed FODMAPs are thought to directly upset the bacterial balance in our gut. In line with this theory, regular probiotic supplementation has been shown to effectively reduce symptom severity in IBS patients. I suspect that the addition of probiotics to a low FODMAP diet will be very beneficial.
A low FODMAP diet plan and dining out ideas

Diet plans are generally tailored to individual patients as we all have different eating habits and preferences.
However I have put together a sample 7-day diet plan that you can see here in more detail.
There are also pre-packaged foods formulated to be low in FODMAPs if you prefer the convenience.
For example, Fodmapped products is the world’s first dedicated FODMAP brand and is available for sale in Australia, the UK and more recently, the US.
Here is a low FODMAP food list of common products found worldwide.
Low FODMAP dining out ideas

Set meal plans aren’t particularly useful when you’re eating out at a restaurant or takeaway shop. Here are some food choice tips to help you make appropriate choices:
- Café: choose tea or coffee with lactose-free or almond milk, poached eggs on sourdough or gluten free bread with grilled low FODMAP vegetables, lactose-free yoghurt with low FODMAP fruit (Greek yogurt or quark is okay too but still has some lactose), smoothies made with lactose-free or almond milk and low FODMAP fruits and vegetables
- Pub food: choose plain meat, chicken and fish with low FODMAP salad or vegetables, olive oil and lemon juice as a dressing, fries with plain salt
- Asian: choose stir fries with no onion or garlic, sushi, sashimi or rice paper rolls
- Mexican: ask for no onion, garlic, beans and sour cream on corn nachos or tacos
- Italian: choose gluten free pasta and ask for an accompanying sauce that does not contain onion or garlic, or ask for a salad with plain meat or chicken with olive oil and lemon juice as a dressing
- Fast food: choose fries with plain salt
- Cinemas: choose popcorn and water
Summary: At the beginning of a low FODMAP diet it’s much easier if you prepare your own meals at home, just to get familiar. And while it can seem overwhelming at first, trends start to emerge between what you can eat at home and dining out.
DIY or do I need help from a Dietitian?
As you can see the low FODMAP diet is complex.
This is generalised advice and may be difficult to do yourself without professional guidance.
Group education sessions have recently been used with success, but it’s traditionally done in a one-on-one setting so that any diet modifications are individualized. In fact, the diet has only ever been evaluated formally as a dietitian-delivered diet (12).
For this reason it’s recommended to do this under the guidance of a dietitian where possible.
That said, with the quality of resources now available online it certainly can be done on your own, but you must be highly motivated and disciplined.
I recommend you to buy the Monash University Low FODMAPs app (we have no affiliation). Monash is the world’s leading source of FODMAP research and information (from Melbourne, Australia), and their app is worth every penny.
Consider probiotics as well either before you start the FODMAP diet or after you have finished. Also speak with your doctor or dietitian first just in case you require medication.
Safely removing and reintroducing the appropriate foods takes a lot of learning upfront, but countless patients can tell you it’s worth it.
Would you like personalized support with this?
We offer a concierge-level service where we walk clients through the entire gut healing process, from the nutrition to the behavior and psychology and more.
This is a premium service we’ve been running since 2019 and I’m confident it’s the absolute quickest way to resolve symptoms and heal your gut in a sustainable way.
To apply with us please fill in this form and schedule a nutrition assessment call with one of our specialists, where we can determine if we can help you and explain what options are available.
The “What Can I Eat on a FODMAP Diet?” food list
This is a giant list of what foods to eat, and what foods to avoid when following a low FODMAP diet.
This is how it looks:
You can download a large and printable 4-page PDF version now by tapping the blue button below:
Frequently Asked Questions About The Low FODMAP Diet
What protein powders are low FODMAP?
Whey protein isolate (WPI) is low FODMAP at 40 grams. Whey protein concentrate (WPC) may not always be low FODMAP depending of the lactose content.
Rice and pea protein are vegan protein powders that are low FODMAP at 40 grams (2 tablespoons).
Just also check that the protein powder doesn’t contain any other high FODMAP ingredients.
For more detailed information on picking a low FODMAP protein powder see this article.
Can I still do The Low FODMAP Diet if I’m a Vegetarian or Vegan?
Yes of course, but it can be more tricky because many staple vegetarian and vegan protein options are high FODMAP.
This includes legumes, some nuts and soy products.
Low FODMAP vegetarian and vegan protein options include:
- Firm tofu (2/3 cup cubed, 160g)
- Tempeh (100g)
- Quorn mince, no onion (75g)
- Eggs (2 eggs, 117g)
- Some nuts and seeds (refer to this low FODMAP food list for specifics)
- Canned and rinsed chickpeas/garbanzo beans and butter beans (1/4 cup, 42g)
- Canned and rinsed lentils (1/2 cup, 46g)
- Quinoa (1 cup cooked, 155g)
- Soy protein milk (1 cup, 250ml)
- Lactose free cow’s milk (1 cup, 250ml)
- Lactose free yogurt (1 tub, 170g)
- Greek yogurt (4/5 cup, 200g)
- Hard yellow cheese e.g. cheddar, Colby, Swiss (2 slices, 40g)
- Cottage cheese (4 tablespoons, 36g)
- Soy cheese (2 slices, 40g)
Can I Cook With High FODMAP Foods and Then Just Remove Them?
Yes and no. Let’s start with the no.
Unfortunately, most FODMAPs mix with water (known as water soluble). This means mixing high FODMAP foods with other ingredients when cooking could see the FODMAPs leach into the low FODMAP food (virtually every other ingredient or food contains water). Cooking with garlic and onion is the main example when this occurs.
It’s thought that high temperature cooking can breakdown FODMAPs (potentially favorable), but to what extent is not yet known. Therefore, currently the best way to keep your meal low FODMAP is to cook with only safe ingredients.
There is an exception, which is why I said “yes” in the beginning.
Cooking with garlic and/or onion in oil is safe as long as you remove all pieces before you add any other ingredients. While FODMAPs mix with water, they do not mix with oil (much like water does not mix with oil, if you ever drop oil into water you will see).
So for example, you can cook whole garlic cloves in oil, which allows the flavor compounds to mix with the oil but not the FODMAPS. Then remove the garlic from the oil before adding any other ingredients (so keep the garlic pieces large so they are easy to remove). This leaves you with what is essentially garlic-infused oil, which is low FODMAP.
More on IBS, FODMAPs and related topics
- Best Remedies, Medicine, & Low FODMAP Products For Stomach Pain and IBS
- 7-Day Low FODMAP Diet Plan For IBS
- FODMAP Reintroduction Plan and Challenge Phase: Your Guide and FAQ
- The “Eat This, Not That” FODMAP Foods List
- Best Probiotics For Irritable Bowel Syndrome (IBS): Explained in Plain English
- How To Stop Diarrhea: Diet Changes and Natural Remedies
- 11 Warning Signs You Have A Sneaky Food Intolerance