Many people claim to have “cured” ulcerative colitis with diet or supplements.
Unfortunately, there is no diet or pill that can cure the disease.
However, certain diet changes have shown tremendous promise in reducing symptoms and easing discomfort, helping patients live a normal life once more.
This article explains what we currently know about the role of diet in ulcerative colitis.
What is Ulcerative Colitis?
Ulcerative colitis is a chronic type of inflammatory bowel disease (IBD), like Crohn’s disease and microscopic colitis that affects the colon (large intestine).
Recent studies estimate that IBD affects 2 million people worldwide (1).

Ulcerative colitis causes inflammation and sores in the inner lining of the colon. Inflammation often begins in the rectum, but it can spread throughout the large intestine.
Summary: Ulcerative colitis is a type of inflammatory bowel disease that causes inflammation and sores in the colon.
Ulcerative Colitis Symptoms and Causes
Ulcerative colitis is thought to develop when a person at genetic risk is exposed to certain environmental stressors.
These environmental stressors either change the ratio of gut bacteria or alter the way the immune system responds to bacteria (2, 3).
As a result, the immune system attacks the intestinal lining causing inflammation and other symptoms, including:
- Abdominal pain
- Diarrhea (often with blood, pus or mucus)
- Nausea
- Poor appetite
- Fatigue
- Frequent bowel movements or urgent need to go
- Weight loss
- Fever
- Anemia (low red blood cell count)
- Leaky gut (increased intestinal permeability).
What Causes Ulcerative Colitis?
The same environmental factors that contribute to disease onset can also cause debilitating flares.
Certain medications are known to increase disease risk and trigger flares. You should speak with your doctor to learn if any you use are relevant to your risk.
Stress is also thought to be a major contributor, as well as diet (4, 5).
In particular, research has linked excessive use of sugar and artificial sweeteners to IBD, but other studies have shown no connection (2, 6).
Some research has also shown a strong link between animal protein and IBD risk.
For example, in an observational study of more than 67,000 middle-aged French women, those who frequently ate meat and fish were significantly more likely to develop IBD. Eggs and dairy were not linked to increased risk (7).
Summary: A combination of genetic, environmental and immunological factors contribute to ulcerative colitis risk. Symptoms occur in flares and include digestive complaints, as well as fatigue and fever.
Would you like more information on how to start a low FODMAP diet for colitis?
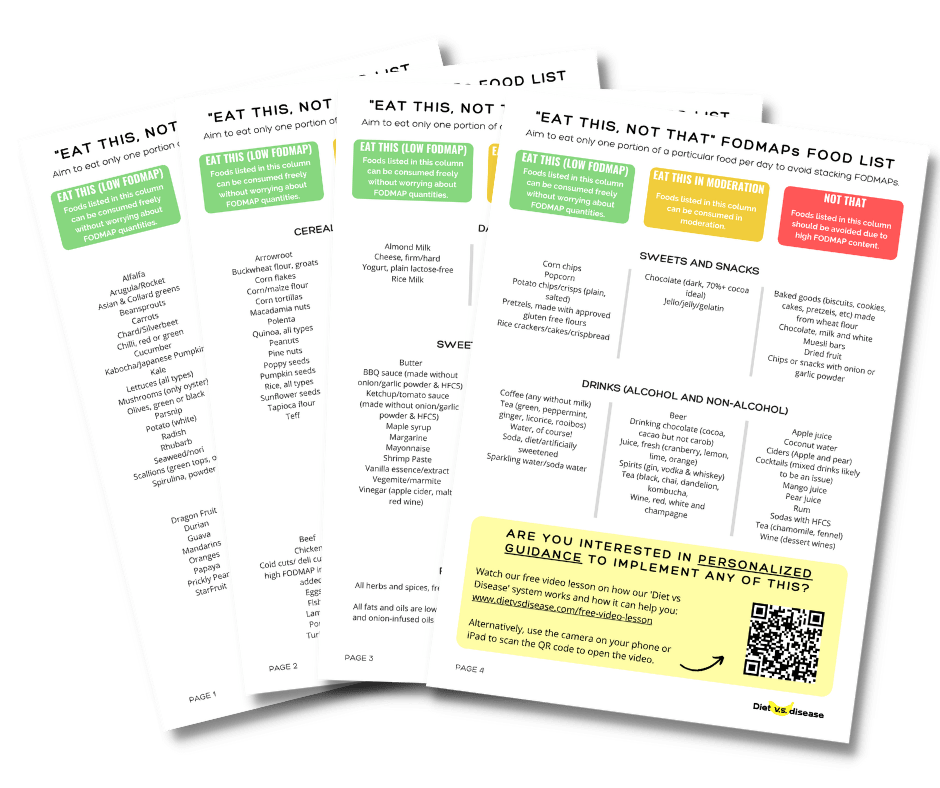
Tap the blue button below to download our “Eat This, Not That” list as well as additional resources for IBS and ulcerative colitis (it’s free!)
What to Do During a Flare

Medications are typically used to manage flares and induce remission as quickly as possible.
In addition, certain diet changes may help shorten flares. Some tips to keep in mind:
- Keep a food and symptom journal during flares to identify bothersome foods. This also ensures that foods are not avoided without cause.
- Eat small, more frequent meals as opposed to 3 large meals in a day (8).
- Ask your doctor whether to limit fiber until symptoms pass. Eating a maximum of 10 grams of fiber per day may reduce irritation and lower the risk of intestinal blockage. Once you are in remission, gradually increase your fiber intake, depending on how much you can tolerate, until you reach the recommended daily intake of 25–30 grams.
- Drink plenty of fluids to avoid dehydration.
Foods to Avoid
Different foods will trigger different people, but its best to avoid these foods to start:
- Dairy: This one is controversial as long-term IBD sufferers tend to have an increased need for calcium. But anecdotal evidence indicates that cutting lactose can help in the beginning, and there can also be emulsifiers in milk that may be problematic.
- Fatty meats
- Caffeine
- Alcohol
- Carbonated beverages
- High-fiber foods, like beans and legumes
- Nuts or crunchy nut butters
- Popcorn
- Chocolate
- Refined sugars
- Spicy foods (6, 9, 10).
Summary: Diet changes during flares can support medications to bring on remission faster. Some find it helpful to avoid fatty foods, caffeine, alcohol and high-fiber foods.
Can Elimination Diets Cure It?
Up to 60% of IBD patients have tried an elimination diet to relieve ulcerative colitis symptoms (12).
Unfortunately, the only known cure is total surgical removal of the colon and rectum (13).
There is no scientific proof that any diet can cause remission on its own. However, limited evidence suggests that certain diets can greatly improve comfort and quality of life.
The impact of diet on inflammatory bowel disease. Click to enlarge. Image source.
Specific Carbohydrate Diet
The Specific Carbohydrate Diet (SCD) has long been reported to relieve symptoms of ulcerative colitis.
It limits complex carbohydrates and eliminates refined sugar and lactose. It’s believed that these foods travel to the bowel undigested, where they alter gut bacteria and cause discomfort (2).
Foods permitted on the diet include most fruits and vegetables (except canned produce and starchy vegetables), meats, certain legumes, honey and lactose-free dairy products.
GAPS Diet, IBD Anti-Inflammatory Diet and Paleo Diet
The GAPS (Gut and Psychology Syndrome) Diet, the IBD Anti-Inflammatory Diet (IBD-AID), and the Paleo Diet are all similar in that they exclude most grains. The Paleo Diet eliminates all dairy products, too (14).
The IBD-AID includes prebiotic and probiotic foods and a specific ratio of healthy fats. It also permits oats.
Small studies have shown the IBD-AID (and SCD mentioned above) to improve IBD symptoms. Larger, more well-designed studies are needed to better determine if there is a role for these diets in IBD treatment (14, 15, 16).
Conversely, the Paleo Diet and the GAPS Diet have not been proven to be beneficial in ulcerative colitis.
The removal of grains in particular is questionable for IBD. Several studies have shown cereal grains to be helpful in reducing ulcerative colitis symptoms and protecting against flares.
In one study, 22 ulcerative colitis patients in remission ate 60g of oat bran per day for 3 months. Fecal studies after treatment showed a significant increase in butyrate, a short-chain fatty acid that is known to heal the intestinal wall (17).
Another study of 18 patients showed that 20–30g per day of germinated barley foodstuff increased beneficial gut bacteria and butyrate, and reduced symptoms (18).
Patients in both studies ate grains without discomfort.
Low FODMAP Diet

The low FODMAP diet is an elimination diet that’s shown promise in managing irritable bowel syndrome (IBS) (19).
It restricts short-chain carbohydrates for several weeks then reintroduces them to see which foods cause digestive problems.
In one study of 72 IBD patients who’d received low FODMAP diet education, those who successfully followed the diet for 3 months reported significant reduction in abdominal pain, bloating and diarrhea (20).
Other studies have shown mixed results for ulcerative colitis.
It’s believed the disease doesn’t cause FODMAP sensitivity but that there is an overlap between the two conditions. Any benefit seen in IBD may be from a reduction in functional digestive symptoms (20, 21).
One concern with the low FODMAP diet is that it limits vegetables and prebiotic foods, both of which are thought to protect against IBD (12, 23).
It’s important to note that the low FODMAP diet should not be followed long-term. FODMAPs must be reintroduced to the diet to some extent.
Keeping the elimination period to a few weeks and working with a registered dietitian can help maximize the benefits of a low FODMAP diet while reducing the risk of nutrient deficiencies.
Low-Residue Diet
A low-residue diet limits your fiber consumption to around 10 to 15 grams per day.
Essentially, you’re free to eat a variety of foods, as long as you keep your fiber intake down.
Foods should be easy to digest and can include dairy, refined grains (with less than 1/2 a gram of fiber per serving), meats, fish, eggs, fruits (except bananas) and most vegetables.
While a low-residue diet is often recommended during flares, there’s no evidence that supports its relief in symptoms. In fact, it could potentially lead to further gut flora imbalance (24).
Semi-Vegetarian
A semi-vegetarian diet limits meat, fish and poultry intake and includes fruits, vegetables, grains, eggs, dairy and legumes.
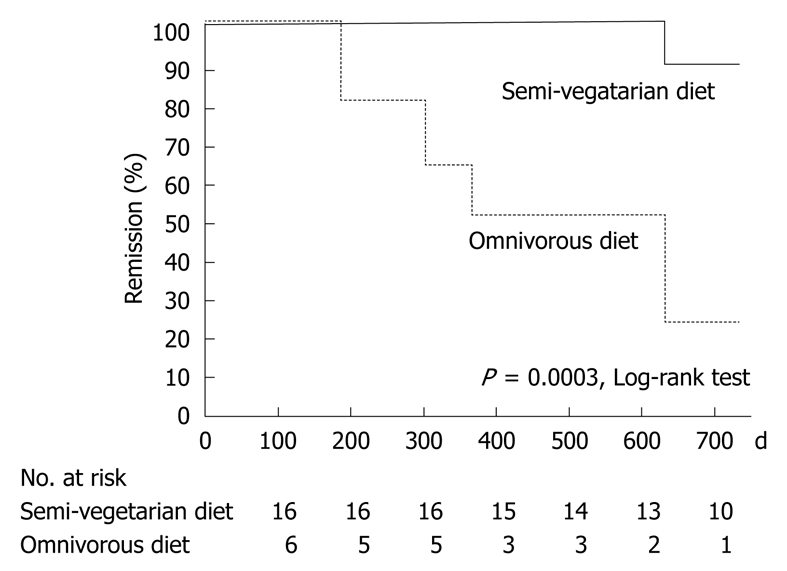
In one study, 22 patients in remission from Crohn’s disease were given educational materials about a plant-based diet that allowed fish once per week and meat every two weeks.
Sixteen patients were able to follow the semi-vegetarian diet for 2 years. The treatment group was significantly more successful in maintaining remission than those who resumed eating meat (25).
Comparison of remission rates over time for the semi-vegetarian group and those who returned to a standard diet. The top line represents the semi-vegetarian diet, with 100% of semi-vegetarians maintaining remission for more than 600 days. Click to enlarge. Image source.
The semi-vegetarian diet has not been studied in ulcerative colitis patients. Clinical trials are needed to determine if it may be beneficial.
However, given newer evidence linking high meat intake with ulcerative colitis, it’s likely to become a research focus.
Maker’s Diet
The Maker’s Diet (also called the Bible Diet) allows only unprocessed and organic foods and specific supplements.
It’s become a popular topic in online IBD support forums because its creator claims the diet cured his Crohn’s disease.
There have been no studies on the diet to date. The United States Food and Drug Administration issued a warning about the supplements, which are sold through the diet creator’s website.
It’s best to be wary of any diet that claims to be a cure, especially when it comes with pricey supplements.
Summary: No elimination diet has been proven to cure ulcerative colitis. Many popular diets limit foods that may in fact be beneficial. Low FODMAP and semi-vegetarian diets show some promise, but larger studies are needed on these meal plans.
Probiotics and Other Supplements for Ulcerative Colitis
Many supplements are advertised to help with ulcerative colitis symptoms.
However, strong evidence is lacking for most supplements, with the exception of probiotics.
Always check with your doctor before beginning any new supplement.
Probiotics
Probiotics are bacteria that offer health benefits by helping to restore the balance of microflora in the gut. They’re found in dairy and fermented foods and are also available in supplement form.
Fecal studies have shown that the composition of gut bacteria in those with ulcerative colitis is very different to that in healthy people, so probiotics may be helpful for correcting the imbalance.
The bacteria strains Escherichia coli (E. coli) Nissle 1917 and Lactobacillus rhamnosus GG have been shown in small studies to be as effective as aminosalicylate medications in maintaining remission in ulcerative colitis (25, 26, 27).
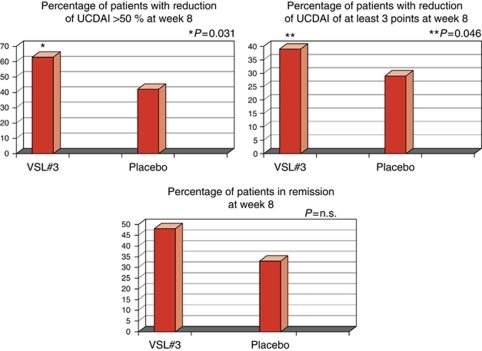
Also promising is the probiotic blend VSL#3. Studies have shown VSL#3 to be as effective as standard medications in bringing about and maintaining remission and reducing symptoms (28, 29, 30).
In a double-blind study, one group of 65 symptomatic ulcerative colitis patients took VSL#3 at a dose of 3600 billion colony-forming units (CFU) per day for 8 weeks. A second group of 66 ulcerative colitis patients received a placebo. All participants received standard ulcerative colitis medications during the study.
Participants recorded their symptoms in a diary, and researchers assigned each participant a score on the Ulcerative Colitis Disease Activity Index (UCDAI) at the beginning and end of the study.
Disease activity score was reduced by a much greater margin for the VSL#3 group compared to the placebo group at 8 weeks. They also showed significant improvements in rectal bleeding and were more successful in maintaining remission at 8 weeks (30).
Comparisons of VSL#3 and placebo in reduction of Ulcerative Colitis Disease Activity Index (UCDAI) score and remission rates. The first chart shows the difference between VSL#3 and placebo in those with a 50% or greater reduction in UCDAI score, while the second shows the difference between VSL#3 and placebo in improving UCDAI score by at least 3 points. Higher percentage is better for all charts. Click to enlarge. Image source.
However, ongoing treatment may be key with VSL#3, as one study found that beneficial bacteria returned to pre-treatment levels within 15 days of discontinuing use (2).
Probiotics are safe for most people but can be very expensive. Ask your doctor for a recommended strain and dose if you wish to try them.
Prebiotics
Prebiotics are fibers that feed the good bacteria in the gut.
Food sources include leeks, Jerusalem artichokes, garlic, chicory root, onions, bananas, apples, barley and oats.
Germinated barley foodstuff and psyllium husk are both known to increase butyrate production. Butyrate helps to repair the intestinal wall and reduce inflammation (18, 31, 32, 33).
In one study of 105 ulcerative colitis patients in remission, psyllium was nearly as effective as aminosalicylate medications at maintaining remission for 12 months. Remission rates in the study were highest when psyllium and medications were taken together (33).
And the prebiotics inulin and oligofructose have been shown to increase two types of beneficial bacteria (Lactobacilli and Bifidobacteria) in the gut. One small study showed that oral inulin supplements that were enriched with oligofructose decreased concentrations of inflammatory proteins in the feces (34).
Both the psyllium and inulin studies reported good patient tolerance. More research is needed to determine if prebiotics are safe and effective for ulcerative colitis.
I’m also weary of garlic and onion, which are very high in a FODMAP called oligosaccharides. This is known to cause digestive issues in a lot of people who are sensitive so I’d be looking at other prebiotic sources.
L-Arginine and L-Glutamine
L-arginine and L-glutamine are amino acids that are used to build proteins.
They are made in the body, although sometimes not in sufficient amounts. They can also be found in meat, dairy and certain grains.
Both of these amino acids are known for their anti-inflammatory properties. Glutamine is said to be helpful in healing leaky gut syndrome, although this is questionable.
Arginine has been shown in rodent studies to heal wounds and reduce inflammatory chemicals in the blood (cytokines) (35, 36, 37).
However, results from human studies are less clear.
Blood arginine levels in one small study were linked to more severe ulcerative colitis. But researchers suspect that ulcerative colitis patients may not be able to take up arginine into the cells effectively. In other words, some patients have high arginine levels overall but not enough usable arginine (38).
More human studies are needed.
Herbal Therapies

Studies have linked several herbal supplements to reduction of ulcerative colitis symptoms.
Some show promise at inducing remission and improving symptoms. However, few studies have established safe and effective doses.
- Aloe vera gel is taken from the leaves of the aloe plant. It’s known for its strong anti-inflammatory properties.
In a trial of 44 patients with active ulcerative colitis, 200 milliliters (mL) per day of aloe vera gel for 4 weeks reduced symptoms more significantly than placebo.
Aloe vera is considered safe for most people (39). - Wheatgrass (Triticum aestivum) is a form of grass that is available fresh or as a powder, juice or tablet.
In one study of ulcerative colitis patients, a group of 11 patients drank 100 mL of wheatgrass juice daily for 1 month. A second group of 12 patients received a placebo drink.
The wheatgrass group had significantly less rectal bleeding and greater improvements in disease activity than the placebo group.
Wheatgrass is generally safe but may cause mild nausea (40). - Andrographis paniculata is an Asian herb that is available as a capsule.
Studies have found it brings about remission faster than placebo and at a comparable rate to aminosalicylates.
The doses in these studies ranged from 1200 milligrams (mg) to 1800 mg per day for 8 weeks (41). - Xilei-san is an anti-inflammatory Chinese herbal blend that’s given as a suppository or enema.
It’s believed to be comparable to standard topical medications and significantly better than placebo in reducing inflammation and bringing about remission (42, 43).
Because it’s delivered in enema or suppository form, it’s most effective for lesions and inflammation in the rectum. - Curcumin is reported to have anti-inflammatory, wound-healing and antispasmodic properties. It’s the active ingredient in the spice turmeric.
In one study of 99 ulcerative colitis patients in remission, curcumin was much more effective than placebo in reducing inflammation and lesions and in maintaining remission (44).
But a large review of curcumin released recently showed that its effects may be overstated. The authors reviewed more than 120 clinical trials and found no strong evidence to support its use. In fact, they believe that the herb may mask inflammation rather than heal it (45). The authors acknowledge that the herb may be found to be beneficial down the road. But more research is certainly needed in light of this new study.
Summary: Many supplements claim to bring about or maintain remission. But specific probiotic strains are the only supplements that have strong scientific support at this time.
Specific Foods and Nutrients
Just as some foods are known to increase risk for ulcerative colitis, others are thought to have protective effects.
Fruits and Vegetables

High fruit and vegetable intake appears to protect against ulcerative colitis. Certain types may even reduce symptoms during flares.
Fruits and vegetables are high in fiber, which is thought to lower risk for IBD. Many are also high in antioxidants, which help to repair and protect the body’s cells (46).
High vegetable intake was linked to lower risk in a review of 19 studies that included 1340 ulcerative colitis patients. A second review of 14 studies found lower rates of the disease in people who ate large quantities of fruits and vegetables (47, 48).
It’s been suggested that citrus fruits and black raspberries may be especially helpful.
One study of 398 ulcerative colitis patients and 616 controls found higher disease rates in those with low intake of citrus fruits. It was not clear whether citrus fruits alone protect against the disease, or if those who eat more citrus simply have higher quality diets. More research is needed (49).
And a study of mice with experimental colitis found that a diet consisting of 5% of calories from black raspberries protected against ulcers (50).
Many fruits and vegetables contain FODMAPs, and some people with ulcerative colitis may find that certain types cause digestive symptoms.
Patients with pain, gas or bloating during remission may wish to work with a dietitian to identify any FODMAP sensitivities. And some may find it helpful to avoid higher-fiber fruits and vegetables during flares.
Dietary Fats
Research on dietary fats and ulcerative colitis is murky, with results from different studies seeming to contradict each other.
The disease has been associated with high intake of all forms of dietary fat. But some studies suggest omega-6 fatty acids increase risk while omega-3 fatty acids are protective (48, 51).
Some of the richest dietary sources of omega-3 fats come from fish. But animal protein, including fish, is linked to higher rates of disease (7).
Studies have also shown that omega-3 supplementation does not lengthen remission or decrease need for medications (52).
It’s not yet known if plant sources of omega-3 fatty acids increase risk. Non-meat sources include flax and chia seeds, walnuts, omega-3 enriched eggs, and leafy greens. Use caution with seeds, as they may irritate the colon during flares.
Vitamin D

Vitamin D deficiency is common in IBD.
One study from the Netherlands found that 82% of IBD patients are low in vitamin D, compared to 31% of healthy adults (53).
It appears to be important in IBD prevention because it regulates the immune system and maintains the intestinal barrier (54, 55).
One study of Crohn’s disease patients found that 2000 international units (IU) per day of vitamin D is helpful in reducing intestinal permeability and inflammation (56).
But very high doses may cause more harm than good. One rodent study found that high doses of vitamin D during flares decreased bone density.
Mice in this study received up to 5000 IU/kg of vitamin D per day. The estimated human equivalent is 3648 IU/60 kg. So a person weighing 68 kg (150 pounds) may see the same effect at 4145 IU per day (57, 58).
Summary: Fruits and vegetables appear to protect against ulcerative colitis and should be eaten as tolerated. The role of omega-3 fatty acids and vitamin D is less clear. Safe upper limits for ulcerative colitis patients have not yet been established.
An Ulcerative Colitis Diet: Summarizing The Evidence
Despite many reports online that certain diets or supplements can cure ulcerative colitis, the only known cure is total removal of the colon and rectum.
Those with digestive symptoms during remission may find relief from a low FODMAP diet to identify trigger foods.
A semi-vegetarian diet has also shown promise in maintaining remission in Crohn’s disease and may be helpful for ulcerative colitis, but we cannot make firm conclusions.
Even without following elimination diets, certain patterns have been shown to reduce symptoms:
- A diet that is rich in fruits and vegetables provides fiber and antioxidants, which are linked to lower disease risk. Reducing intake of high-fiber fruits and vegetables may increase comfort during flares.
- Limiting dietary fat, especially fatty meats, may be beneficial.
- Certain probiotics are helpful in bringing about and maintaining remission. Ask your doctor for a recommendation.
- A few herbal supplements show promise but lack sufficient scientific evidence to support their use.
- Avoid foods that irritate the gut during flares, including fatty foods, caffeine and alcohol.
A registered dietitian can help you identify foods that trigger your symptoms and design a well-balanced meal plan.
Would you like more information on how to start a low FODMAP diet for ulcerative colitis?
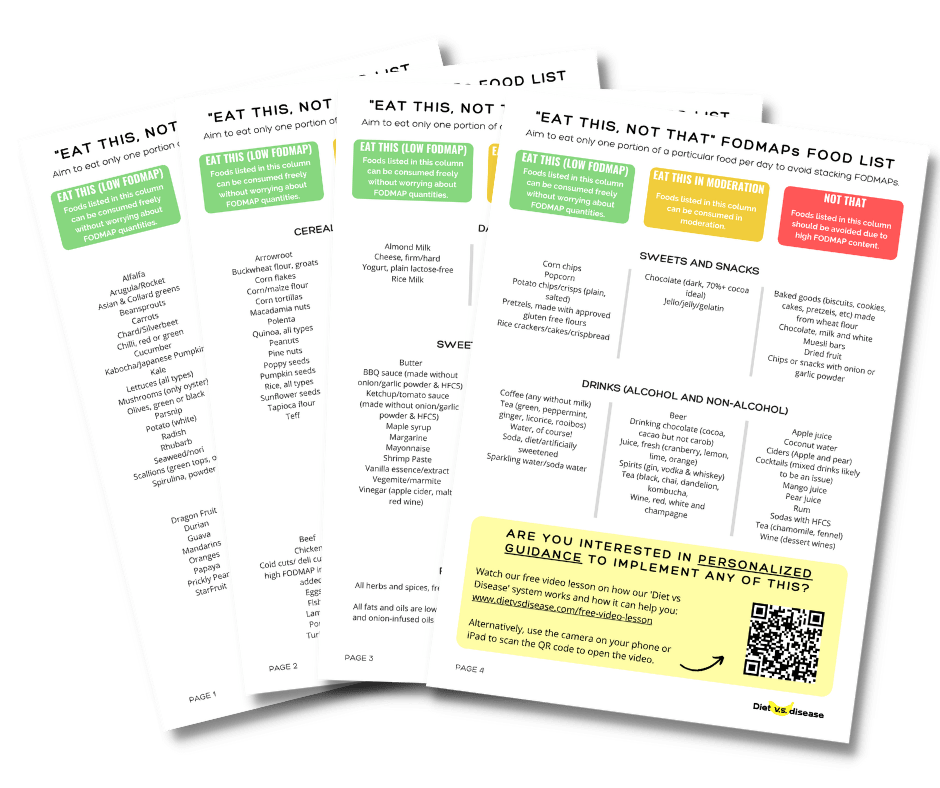
Tap the blue button below to download our “Eat This, Not That” list as well as additional resources for IBS and colitis (it’s free!)