Histamine intolerance is poorly understood in the medical world.
Most health professionals are not knowledgeable on the topic; diagnosis is flaky at best; and the condition itself is difficult to treat.
That’s why I’ve created this guide. It’s a comprehensive, research-driven review of histamine intolerance, with a particular emphasis on diet and treatment.
What is histamine? A simple definition
Histamine is a chemical that is both made by the body and found naturally in certain foods.
In the body it’s produced by mast cells (a type of white blood cell) and has a crucial role in our immune system. It’s actually the key mediator in causing the symptoms of allergy, which is why we take antihistamines for allergy relief.
Histamine also occurs in our food as a by-product of the fermentation of Histidine, which is a form of protein. In this context it’s part of a family of chemicals known as Biogenic Amines, which are produced by bacteria during fermentation, storage or decay (1, 2).
While high levels of biogenic amines (such as histamine) can make you feel unwell, the majority of people tolerate the amounts found in a regular diet.
Summary: Histamine is a chemical that has a crucial role in our immune system. It’s produced by the body and also found in certain foods.
What is histamine intolerance?
Approximately 1% of the population experiences adverse reactions to what is considered a “normal” level of histamine in food (3).
This increased sensitivity is called a Histamine Intolerance.
It develops through both increased availability of histamine in the body, and decreased activity of the enzymes that break down histamine and remove it from your system. This “defect” is primarily thought to be caused by previous gastrointestinal disease and/or genetics.
The main histamine enzyme in the gut is Diamine Oxidase (DAO), while areas like the skin, spinal cord, lungs and other organs rely on an enzyme called Histamine N-Methyltransferase (HNMT) (3).
So, an individual with a histamine intolerance will have low levels of DAO or HNMT (or both), which can lead to a build-up of excess histamine in their blood plasma.
It’s not unlike those with a FODMAPs intolerance, or those intolerant to caffeine or lactose. These conditions are also the result of enzyme problems.
What can cause high histamine levels?
Some reasons why you may have lower levels of DAO and higher levels of histamine include:
- Certain medications that block DAO production, including several antibiotics
- Gastrointestinal disorders like leaky gut syndrome and inflammatory bowel disease
- High histamine foods and foods that trigger histamine release (see list below)
- Bacterial overgrowth, like that found in SIBO
Histamine levels and testing
Normal levels of plasma histamine range from 0.3–1.0 ng/mL, but anything above this causes problems.
For example, a level of 1–2 ng/mL can increase stomach acid secretion and heart rate, while levels of 3–5 ng/mL can cause flushing and headaches (4).
A histamine-sensitive individual who consumes a high histamine meal is likely to get high plasma histamine levels. Unfortunately, there are no common tests to diagnose this, and the skin prick test is fairly new (5).
Therefore, it’s important that an experienced clinician rules out food allergies before tweaking your diet for histamine intolerance.
Summary: An increased sensitivity to histamine is called a histamine intolerance. It develops through both increased availability of histamine in the body, and decreased activity of the DAO enzymes that break it down. This can be caused by certain medications, gastrointestinal disorders and/or high-histamine foods. There are no common tests to diagnose this condition.
Get Our “Eat This, Not That” Histamine & Food Chemicals Food List
This is our unique list of what foods to eat and what foods to avoid when following a low histamine diet, which is low in food chemicals. This is how it looks:
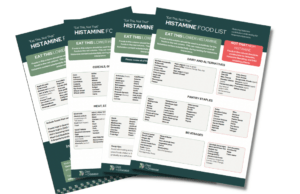
You can download a large and printable 4-page PDF version now by tapping the blue button below:
Signs and symptoms of histamine intolerance
While symptoms appear allergy-like, they do not involve an IgE-mediated response and therefore are not allergic reactions (hence the term intolerance).
Of course, there is no way to know this until you have ruled out allergy through tests.
The onset and severity of histamine intolerance symptoms vary greatly between individuals, but common complaints are:
- Flushing and headaches
- Respiratory problems including asthma, runny or blocked nose
- Skin conditions likes rashes, dermatitis, hives or eczema
- Gastro problems such as nausea, reflux, vomiting, abdominal pain, diarrhea
- Dizziness, low blood pressure and irregular heartbeat
Also note that antihistamines may help to relieve symptoms, but only if you do not already follow a low-histamine diet (3).
Summary: Symptoms appear allergy-like, but they do not involve IgE antibodies. The only way to be sure is to get tested for allergies.
High-histamine foods to limit or avoid
If you are histamine intolerant, it makes sense to reduce the amount of histamine you consume.
Unfortunately, it’s difficult to quantify the amount of histamine found in different foods. It varies greatly according to the type of bacteria, food composition, length of time unrefrigerated and conditions for fermentation (6).
As a general rule, high concentrations of histamine are typically found in fermented foods such as bread (effects of yeast), sauerkraut, wine, beer, processed meat and aged cheese.
In addition to histamine-rich food, there is an untested theory that several foods have the capacity to release histamine directly from our white blood cells (7).
This means they could contribute to increased histamine levels, even if that food itself is low histamine.
High histamine foods
There is a lot of conflicting information online and I found many authoritative sites did not provide very comprehensive lists.
Here, I’ve summed up the foods that most experts recommend you avoid:
- Fermented dairy products such as aged cheese, yogurt and quark
- Fermented or pickled vegetables
- Soured foods such as sour cream and buttermilk
- Tinned/canned, cured and processed meats
- Fermented soy products including miso, tempeh and soy sauce
- Green tea, matcha tea, coffee, cocoa, chocolate
- All legumes (including peanuts) and tree nuts (regular nuts)
- Citrus fruits, raspberries, strawberries, bananas, pineapple, grapes, pears and fruit juice
- Avocado, eggplant, spinach, olives, tomato and tomato products (ketchup, tomato juice)
- Vinegar, bouillon and broth
- Smoked fish
- Any alcohol
- Junk foods or drinks that contain artificial colours or flavors.
I strongly recommend you also check out this Histamine Compatibility list (PDF) by the Swiss Interest Group Histamine Intolerance (SIGHI).
It ranks the likelihood of foods to cause symptoms on a scale of 0 to 3 as well as other important tips.
Summary: Foods to look out for are either high in histamine or have the capacity to release histamine from our white blood cells. As a general rule, fermented foods are the most histamine-rich and should be avoided.
How much histamine is safe for those who are sensitive?
Defining a safe threshold level for those with a histamine intolerance is incredibly difficult (8).
Firstly, sensitivity to bioactive amines varies greatly between individuals. Unlike food allergies, which are triggered at first exposure, it’s the cumulative amount of histamine that causes symptoms. What may trigger headaches in one person may have no effect on the other.
Secondly, as mentioned above, certain pharmaceutical drugs inhibit the enzyme DAO from breaking down histamine in the body. This can lead to increased histamine levels over time, especially if they are long-term medications (9).
Some of the more common drugs include alprenolol (for blood pressure) and many forms of antibiotics.
These factors must be accounted for when deciding on individualized dietary changes and how strict they should be.
As a general guideline, a limit of 100 mg histamine per kg in foods and of 2 mg histamine per liter in alcoholic beverages has been suggested, although these are likely too generous (10).
Summary: Individual sensitivity to histamine, as well as the impact of certain pharmaceutical drugs can seriously affect plasma histamine levels. Therefore, defining a safe threshold is very difficult.
Get Our “Eat This, Not That” Histamine & Food Chemicals Food List
This is our unique list of what foods to eat and what foods to avoid when following a low histamine diet, which is low in food chemicals. This is how it looks:
You can download a large and printable 4-page PDF version now by tapping the blue button below:
A low-histamine diet

A low-histamine diet is a structured program that’s best done under the supervision of a dietitian specializing in food intolerance.
Once food allergy has been ruled out, the elimination phase involves strictly limiting the amount of histamine you consume for 2-4 weeks. Diet and symptoms must be recorded in your own food diary, which is proven useful in tracking significant improvements and relapses.
The reintroduction phase is next, where you gradually reintroduce histamine-containing foods to determine your tolerance and threshold. It doesn’t need to be done in a particular order, and I generally advise that you reintroduce the foods you miss the most first.
Some pointers to keep in mind:
- Try to cook most of your own meals during the elimination phase
- Avoid or limit eating canned foods and ready meals
- Avoid junk foods; food dyes/artificial colors can be major triggers
- Keep your kitchen clean
- Refrigerate vigilantly as histamine forms on food as it spoils.
A low-histamine diet plan
Here’s an idea of what a realistic low-histamine day would look like:
Breakfast: Cereal + milk
Lunch: Fresh Spring (Rice-Paper) Rolls. Avoid using meat or veggies on the high-histamine list.
Dinner: Pan-seared chicken breast (fresh or thawed rapidly) + roast potato and vegetables (not those on high histamine list)
Snacks: 1 apple or peach; cucumber or carrot sticks + cottage cheese
Drinks: Water, herbal tea
Summary: A low-histamine diet requires you to follow a 2-4 week elimination period, followed by a reintroduction phase to determine your histamine threshold. A diet and symptom diary is necessary, and it’s strongly recommended that you see a specialist dietitian during this entire plan.
Important considerations before you trial a low-histamine diet
Significant dietary restrictions can affect nutritional status at any age (11).
Therefore, the risk–benefit ratio must be considered first when contemplating any form of elimination diet. Much like a low FODMAP diet, a low-histamine diet excludes multiple nutrient-dense foods that provide health benefits.
This is why it’s recommended that you follow a low-histamine diet under the supervision of a dietitian specialized in food intolerance.
Not appropriate for young children
Low chemical diets are becoming increasingly popular for young children despite the lack of evidence that they help.
A 2013 case-study review of 74 children placed on an elimination diet (for salicylates) found that almost half experienced harmful side-effects, including nutritional deficiencies, food aversion and eating disorders (12).
Growth rate is highest within the first years of life and a failure to meet this potential can have a long-lasting impact on development and later health (13).
Therefore, chemical elimination diets are only warranted for young children if there is clear-cut evidence it’s helping with symptoms.
Summary: A low-histamine diet can be quite restrictive even though it’s temporary, so consider your nutrition status before you start. It’s not appropriate for young children.
Supplements for histamine intolerance

There is basically one supplement available marketed specifically for histamine intolerance.
It contains DAO isolated from pig kidneys and is designed to supplement the sub-optimal DAO levels of patients with histamine intolerance.
There was one clinical trial that found DAO supplementation helped to reduce the duration of histamine-induced migraines by 30%, but not the intensity nor how often they occur (14). It was reportedly a small study though, and ideally it would be nice to see if the results can be replicated.
The reviews of this particular supplement are interesting, and you can give it a try. Note that the capsules are labelled vegetarian (as you would expect), but the DAO inside is sourced from pork. Highly misleading labelling.
And as always, please consult with your personal doctor before you decide to try any new supplements.
Vitamin C and vitamin B6
Some researchers believe both vitamin C and vitamin B6 supplementation can be beneficial.
Both nutrients are required (cofactors) for DAO activity, so in theory they act as antihistamines by supporting the breakdown of histamine (15, 16).
One trial found that 5 mg of vitamin B6 supplementation daily significantly increased DAO activity in pregnant teenagers, but only those deficient in vitamin B6. It didn’t benefit anyone else (17).
That’s the only scientific proof I could find, and study after study shows that vitamin supplements are basically useless unless you have a clinical deficiency. Your money is better spent on foods naturally rich in vitamin B6 and vitamin C.
Note that if you want to try vitamin C supplements, it’s best to avoid the form called ascorbic acid. It’s typically derived from fermented corn and/or citrus, both not appropriate for histamine intolerance.
Summary: DAO supplementation was shown in one clinical trial to reduce the duration of migraines, but had no effect on frequency or severity of symptoms. In theory, a vitamin C and/or vitamin B6 supplement may help too, but this is not supported by any strong evidence.
Probiotics for histamine intolerance

Probiotics are microscopic bacteria that we get from fermented foods.
They help to restore and maintain the balance of bacteria in the gut, which is linked to varying aspects of well-being including digestive health and even weight loss.
Fermented foods are not an option for someone with a histamine intolerance, which leaves us with probiotic supplementation. Unfortunately the research is thin.
One study found oral intake of two Bifidobacterium strains supressed factors involved in histamine signalling and production, at least in rats (18).
Another study looked at the effects of several probiotic strains on human mast cells in a laboratory setting. Researchers were able to “turn down the dial” on the immune response and minimize histamine release, especially with two strains of Lactobacillus rhamnosus (19).
It seems that if probiotics were to help, they would be most useful in preventing allergic reactions rather than treating symptoms of histamine intolerance. Nevertheless, if you want to try some just be careful about what strains you use. Some strains of Lactobacillus have been shown to increase histamine content, while other strains decrease it (20, 21).
I suggest this probiotic (Lactobacillus rhamnosus) or this probiotic (Bifidobacterium strains) (full disclosure: these are Amazon affiliate links).
Just note that we don’t know the optimal dosage for this condition, nor the long-term side effects (if any), so always consult with your doctor first.
Summary: Early studies on rodents and in test-tubes have shown that certain probiotic strains may help minimize histamine release. The most effective strains are likely to be Lactobacillus rhamnosus or several Bifidobacterium strains, but there is no guarantee they will help.
This is only a guide…
There are a lot of aspects to consider when treating histamine intolerance, particularly when it comes to diet and nutrition.
While I’m a qualified dietitian, this general advice is no substitute for your personal medical professional that knows your medical history.
That being said, if food allergy has been ruled out, avoiding histamine-rich foods as part of a low-histamine diet is the next logical step. Some supplements and probiotics may help, but I would not expect any miracles.
There’s also the possibility of a food intolerance, which you can learn more about here.
Get Our “Eat This, Not That” Histamine & Food Chemicals Food List
This is our unique list of what foods to eat and what foods to avoid when following a low histamine diet, which is low in food chemicals. This is how it looks:
You can download a large and printable 4-page PDF version now by tapping the blue button below: