Fructose malabsorption is a gastrointestinal condition that causes digestive discomfort.
It’s common in sufferers of Irritable Bowel Syndrome (IBS), but can also be experienced in others.
This article looks in detail at fructose malabsorption and explores the scientifically-proven diet changes that can help improve your symptoms.
What is Fructose and Fructose Malabsorption?

Fructose is a simple carbohydrate, or single sugar, found in many plants.
It’s the major sugar found in fruit, which is why it’s sometimes referred to as ‘fruit sugar’. However, it also occurs naturally in honey, wheat and some vegetables.
Fructose can be found in three ways:
- As free fructose.
- Bonded to glucose to form table sugar.
- As part of a fructan. Fructans are multiple fructose molecules joined to one glucose molecule.
When fructose is eaten, it travels to the small intestine where it is absorbed without needing help from digestive enzymes.
Fructose Malabsorption
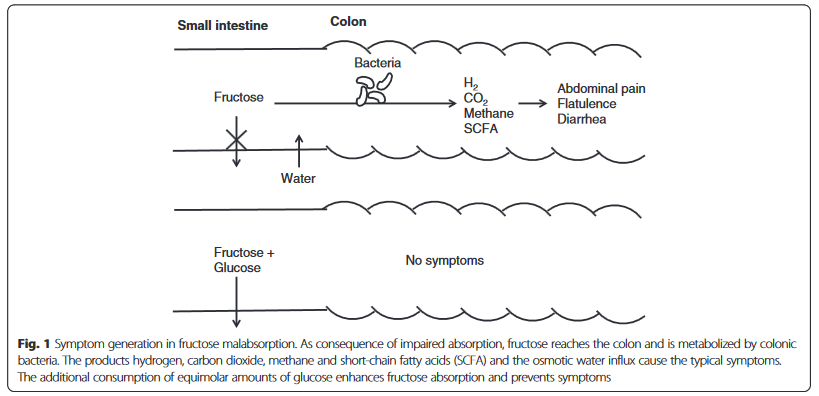
In fructose malabsorption, the left over fructose travels to the colon and takes lots of water with it (called an osmotic effect).
Fructose is then fermented by gut bacteria in the colon (large intestine). This fermentation produces short chain fatty acids and the gases hydrogen, methane and carbon dioxide (1).
Image source. Click to enlarge.
Fructans are slightly different. They always travel straight to the colon where they are quickly fermented by bacteria. When fructans and other fructose are eaten together it may make symptoms worse (2).
Summary: Fructose is a carbohydrate found in many plants. Fructose malabsorption causes fructose to move into the colon where it is fermented by bacteria, producing short chain fatty acids and gas.
Fructose Malabsorption or Fructose Intolerance?

You may hear fructose malabsorption and fructose intolerance used interchangeably, but they may not refer to the same thing.
Fructose intolerance or hereditary fructose intolerance (HFI) is a genetic condition caused by deficiency of an enzyme that breaks down fructose in the liver. HFI is usually diagnosed at a young age, when babies start to eat food or have formula containing fructose (3, 4).
HFI can cause serious liver problems if left unmanaged. Fortunately, like fructose malabsorption, it can be effectively managed with diet changes (5).
Fructose malabsorption is not necessarily genetic, unlike HFI.
Summary: Fructose malabsorption should not be confused with hereditary fructose intolerance. Hereditary fructose intolerance is a genetic condition that prevents the break down of fructose and can cause liver problems.
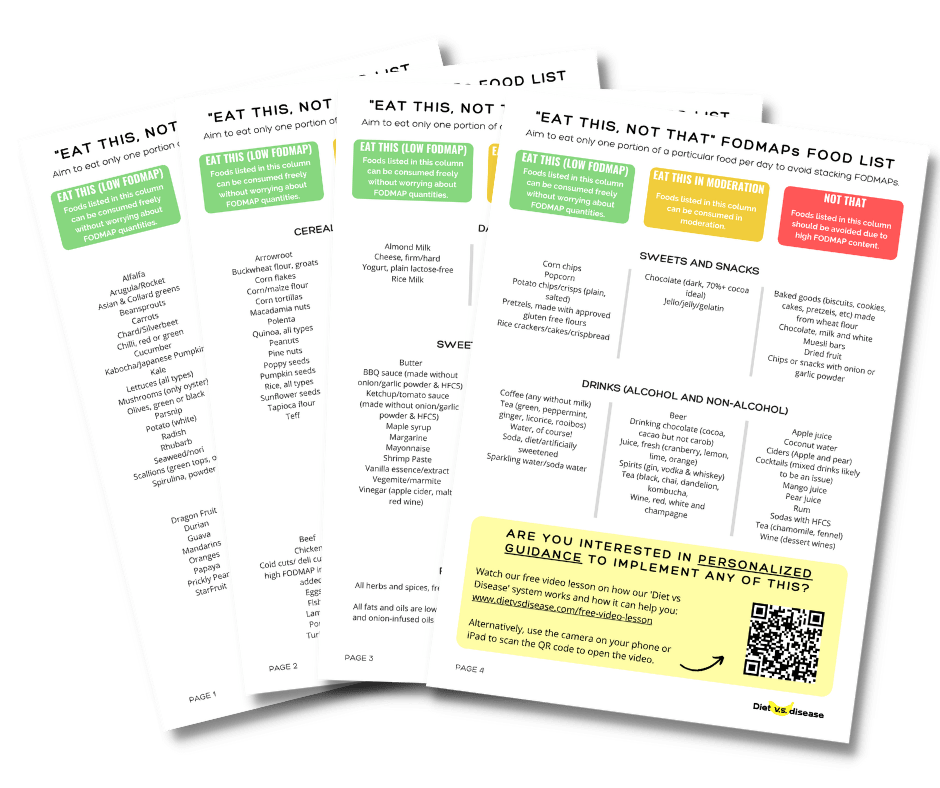
What Can And Can’t I Eat On The Low FODMAP Diet?
Often it’s easiest to start with this giant list I’ve made of what foods to eat, and what foods to avoid when following a low FODMAP diet.
It’s based on the latest published FODMAPs data (1, 2, 3, 4, 5).
Print or save to your phone to use as a quick-reference guide when shopping or cooking. I’ve attempted to list foods in both US and UK/Aus names, with US first.
I’ve included a screenshot of the first page below. But the full PDF is 4 pages and suitable for printing. To download it simply tap the box below and it will then be emailed straight to you – it’s free!
Signs and Symptoms of Fructose Malabsorption

Sufferers of fructose malabsorption often experience similar symptoms to those caused by IBS.
The combination of extra water and gas in the colon is what causes uncomfortable digestive complaints.
Common symptoms include (2, 4, 6):
- Abdominal pain
- Bloating and possibly reflux
- Nausea
- Flatulence
- Diarrhea and/or constipation.
Summary: Symptoms of fructose malabsorption are caused by extra water and gas in the colon. Symptoms include abdominal pain, nausea and diarrhea.
Testing for Fructose Malabsorption
Fructose malabsorption can be diagnosed using a hydrogen breath test (7).
Most of the gas produced by bacteria in the colon moves into the bloodstream and then into the lungs. We then breathe this gas out. The hydrogen breath test measures the amount of hydrogen in our breath (7).
Flow chart for breath testing protocol. Image source. Click to enlarge.
Some people may complete a slightly different test because they naturally don’t produce enough hydrogen gas. In this case, methane gas is usually measured instead (8).
Although the hydrogen breath test is commonly used for diagnosis, some people still experience positive results from diet changes, even when their breath test didn’t show fructose malabsorption (9).
Summary: A hydrogen breath test can be used to diagnose fructose malabsorption.
Diet Changes for Fructose Malabsorption
Eliminating fructose completely from you diet is near impossible.
The main aim is to determine how much you can tolerate without causing uncomfortable digestive issues. Each person is unique.
A low FODMAP diet

A low FODMAP diet is a science-based strategy to determine how much fructose you can tolerate.
People with fructose malabsorption also tend to be sensitive to other FODMAPs too.
FODMAPs are a group of short-chain carbohydrates, like fructose and fructans, which can cause digestive issues when they are poorly absorbed.
The diet involves an elimination phase where you restrict or exclude all FODMAPs for 3-8 weeks. This gives your gut some time to heal and the good gut bacteria time to thrive.
Next, each FODMAP is reintroduced or challenged one at a time. The aim is to learn which FODMAPs you can tolerate and how much of each FODMAP you can eat without having symptoms.
The low FODMAP diet can be quite complicated and difficult to do correctly on your own. I would recommend seeking help from a FODMAP-trained dietitian where possible to achieve the best result.
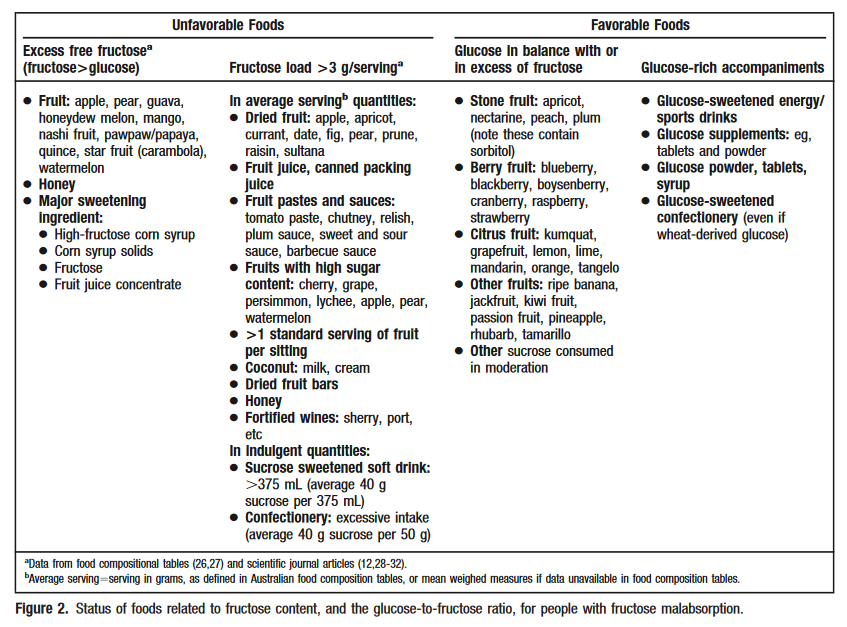
Balance Your Glucose to Fructose Ratio
Glucose is the other main sugar molecule alongside fructose, but they are metabolized differently.
Dr. Sue Shepard and Prof. Peter Gibson, pioneers of the low FODMAP diet, discovered that foods containing as much or more glucose than fructose are better tolerated.
In other words, it helps to eat as much or more glucose than fructose in those who are sensitive (2).
It seems as long as glucose is consumed in a 1:1 ratio with fructose (or greater), the co-transport system will help with fructose absorption in the small intestine (up to a point, it can be overwhelmed) (1, 3).
It’s one of the reasons why foods with excess fructose compared with glucose, such as apples, pears, and mangoes, will likely trigger abdominal symptoms.
Dr. Shepard and Dr. Gibson produced this handy table outlining unfavourable and favourable foods to help make these diet changes.
Favourable vs unfavourable foods related to fructose content. Image source. Click to enlarge.
Summary: A low FODMAP diet can be used to work out if fructose is your only problem and how much fructose you can tolerate. Eating glucose at the same time as fructose can help increase absorption. A registered dietitian can help you create an individualised plan.
Can Supplements Help?
Xylose isomerase

Xylose isomerase is an enzyme that converts fructose to glucose in the small intestine (10).
Taken as a supplement, it may improve symptoms of fructose malabsorption (4, 10).
In a study of 65 patients with fructose malabsorption, patients randomly received a pill containing the enzyme or a placebo. Those that used the enzyme saw significant improvements in abdominal pain and nausea, but not bloating, compared to those that took the placebo (10).
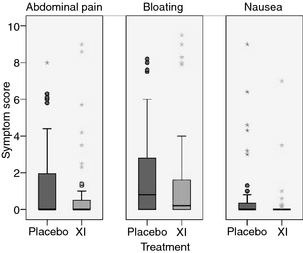
XI = xylose isomerase supplement.
However, patients only had fructose in a water solution. It’s unclear whether the enzyme would act differently, or as effectively, when fructose is eaten as part of a meal.
Other Supplements
Other than xylose isomerase, supplements that help manage overall IBS may also be helpful for fructose malabsorption.
In particular one type of fiber supplement, and potentially probiotics too.
Summary: Xylose isomerase is an enzyme that may reduce fructose malabsorption when taken as a supplement. But much more research is needed.
The Punch Line
Fructose malabsorption is a common condition that is treated with diet changes.
The most important step is to work out how much fructose you can tolerate and how to balance your diet.
A registered dietitian can work with you using a low FODMAP diet and other scientifically tested strategies to eliminate symptoms.
What Can And Can’t I Eat On The Low FODMAP Diet?
Often it’s easiest to start with this giant list I’ve made of what foods to eat, and what foods to avoid when following a low FODMAP diet.
It’s based on the latest published FODMAPs data (1, 2, 3, 4, 5).
Print or save to your phone to use as a quick-reference guide when shopping or cooking. I’ve attempted to list foods in both US and UK/Aus names, with US first.
I’ve included a screenshot of the first page below. But the full PDF is 4 pages and suitable for printing. To download it simply tap the box below and it will then be emailed straight to you – it’s free!