[Last updated 7th March, 2023]
Chronic constipation is a common and uncomfortable complaint.
It’s rarely dangerous and can often be prevented and treated at home with diet and lifestyle changes.
This article explores ten research-backed methods of easing chronic constipation… all of which can be done yourself at home.
Acute vs. Chronic Constipation

Constipation refers to difficulty in moving the bowels.
Most people have experienced acute constipation at least once. It’s caused by many factors, including diet, stress and changes to daily routine, and usually resolves within a couple of days.
Constipation is considered chronic if symptoms are present at least 3 times per week for 3 months. It’s very common and affects up to 27% of the world’s population (1, 2).
Chronic constipation can be caused by medications or health conditions such as thyroid disorders, Parkinson’s disease or spinal cord injuries. Structural and functional problems including slow bowel transit and pelvic floor dysfunction can also cause it.
More commonly it’s the result of irritable bowel syndrome (IBS). Sometimes the cause remains unknown.
This article is largely about chronic constipation.
Summary: Acute constipation is common and usually resolves within days. Constipation is considered chronic when symptoms occur at least 3 times per week for 3 months. This article focuses on chronic constipation.
Constipation Symptoms

It’s a common myth that we must have daily bowel movements to be healthy.
In reality, many people move the bowels only every couple of days. Physicians generally consider fewer than 3 bowel movements per week to be problematic (3).
Symptoms other than bowel frequency are often better indicators of constipation. These include (3):
- Difficulty passing stool.
- Feeling of incomplete evacuation.
- Abdominal pain.
- Bloating.
- Sensation of blockage in the rectum.
- Hard or lumpy-looking stool.
- Reduced quality of life.
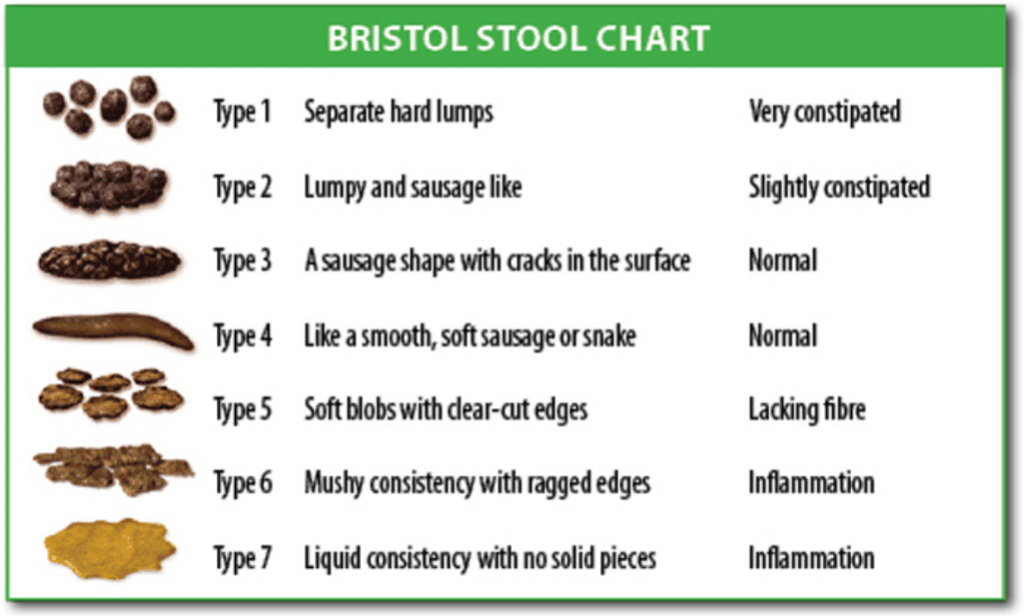
The Bristol Stool Chart is sometimes used in diagnosing constipation.
Types 1 and 2 are the most often seen in constipation (4).
Click to enlarge.
Summary: People with constipation most commonly complain of infrequent bowel movements. But other symptoms — like hard stools, bloating, abdominal pain and reduced quality of life — may be even more telling.
The following 10 tips look at ways of easing or preventing constipation.
1. Treat IBS or FODMAP Sensitivities

Irritable bowel syndrome (IBS) affects an estimated 11% of the world’s population (5).
It causes chronic constipation (IBS-C), chronic diarrhea (IBS-D) or alternating symptoms (IBS-A or IBS-M).
There’s no known cure for IBS, but certain diets including a low-FODMAP diet can help prevent constipation.
FODMAPs are short-chain carbohydrates that are found in many fruits, vegetables, grains, legumes and sweeteners. They’re not digested well in the small intestine and ferment when they reach the bowel, causing constipation and other digestive problems.
Removing high-FODMAP foods from the diet for several weeks and then systematically reintroducing them helps to identify food intolerances. This method has been shown to relieve IBS-C symptoms for those with food sensitivities (6).
More information about a low-FODMAP diet for IBS can be found here.
Summary: Low-FODMAP diets have been shown to help with constipation and other digestive issues. These diets are temporary and are meant to identify food sensitivities.
2. Adjust Your Fiber Intake

Fiber is a type of indigestible carbohydrate that’s found in plant foods.
There are two types of dietary fiber.
- Soluble fiber dissolves in liquids and is found in legumes, nuts, oats and fruits.
- Insoluble fiber is found in the skins and seeds of fruits and vegetables, as well as grains.
The research around whether fiber is beneficial for constipation is a bit confusing. It depends to some degree on the type of fiber, as well as constipation symptoms.
Soluble fiber helps soften and bulk the stool. It has shown better results in reducing constipation than insoluble fiber (7, 8, 9).
In fact, insoluble fiber can worsen constipation for some IBS patients. Lower insoluble fiber intake is advised for those with constipation from slow bowel transit or pelvic floor dysfunction (10).
Incorporating more foods rich in soluble fiber may be useful, but use caution if you’re sensitive to FODMAPs. A registered dietitian can help you plan a low-FODMAP diet that includes adequate soluble fiber.
Some people may find it difficult to reach the recommended 22–30 grams of fiber per day through diet alone. Psyllium (corn husk) fiber supplements may be helpful here. They’re available over the counter in generic form or in products like Metamucil or Konsyl.
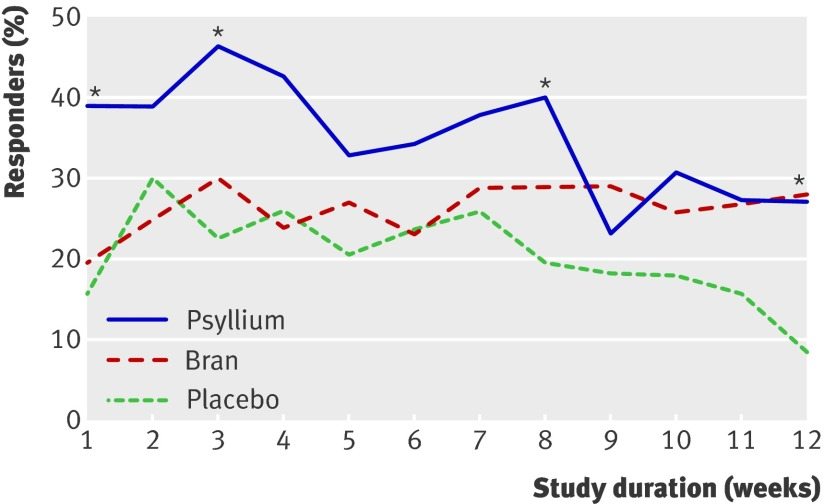
In a clinical trial of 275 IBS patients (including 154 with IBS-C), 10 grams of psyllium fiber per day reduced self-reported abdominal pain and discomfort by a significantly greater margin than equal doses of bran fiber or placebo (7).
Proportion of IBS patients who reported satisfaction with symptom relief over 12 weeks of psyllium, bran or placebo. A higher score is better. Click to enlarge.
Not all IBS patients tolerate psyllium fiber. Starting with a small dose and gradually increasing it may help.
Those who are not FODMAP sensitive may also try prunes or dates. Small studies suggest 100 grams of prunes per day significantly increases stool frequency and consistency.
Prunes are high in polyols, though, and may cause more harm than good in some patients (11).
Summary: The effects of fiber on constipation depend on fiber type and an individual’s symptoms. Soluble fiber has shown more promise than insoluble fiber for symptom relief. Ten grams per day of psyllium fiber or 100 grams per day of prunes may be helpful for some.
3. Drink Adequate Fluids

It seems logical that drinking more fluids would help relieve chronic constipation.
Dry stools are a common symptom, after all.
Surprisingly, studies only show a link between increased fluid intake and prevention of constipation, rather than treatment.
One large study found significantly higher rates of constipation among those who consumed less than 1882 milligrams of liquid per day.
Unfortunately, this study included moisture from both foods and drinks, so it doesn’t clearly tell us how many milliliters of fluid might help prevent constipation. It does, however, show that moist foods (like soups or fruits) may be helpful in addition to drinks (12).
Another small study found that stool frequency and stool weight were significantly lower with intake of less than 500 mL (2 cups) of fluids per day (13).
Of the few studies that suggested fluids were beneficial for easing symptoms, most included other treatments (such as mineral oil or magnesium). It’s difficult to know if the improvements came from drinking more fluids or other factors (14).
All told, there’s not enough evidence to recommend extra fluids as a treatment for constipation. Staying well-hydrated has many health benefits that are not related to digestion, though. Drinking to thirst is recommended.
Summary: Research has not shown strong links between fluid intake and constipation. Small studies show that dehydration may decrease stool frequency and weight, but more research is needed.
4. Probiotics May Help

Probiotics are live microorganisms that are consumed for their health benefits.
Certain strains are helpful in reducing symptoms of IBS, including constipation.
In one study of patients with functional bowel symptoms:
- One group of 33 patients received Bifidobacterium animalis (lactis) at a dose of 17.2 billion colony forming units (CFU) per day.
- A second group of 33 patients received lactis at a lower dose of 1.8 billion CFU per day.
- A third group of 34 patients received a placebo.
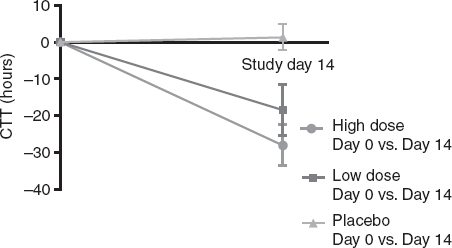
After 14 days, both B. lactis groups showed significantly faster gut transit times on X-ray compared to before treatment, with the greatest improvements in the high-dose group (15).
A comparison of gut transit time from baseline to 14 days for high-dose probiotics, low-dose probiotics and placebo. A lower score is better. Click to enlarge. Image Source.
The groups receiving B. lactis also reported reductions in functional bowel symptoms. Out of 9 symptoms, the high-dose, low-dose and placebo groups showed significant improvements in 8, 7 and 2 symptoms respectively (15).
While this study did not specifically look at constipation, other studies have found B. lactis improves gut transit in those with constipation (16).
In one analysis of previously conducted trials, B. lactis was found to significantly improve stool frequency and consistency, as well as flatulence (17).
Probiotics are safe for most healthy adults. A doctor can recommend a safe and effective dose.
Summary: The probiotic strain B. lactis is thought to be helpful in reducing gut transit time, stool frequency, stool consistency and bowel symptoms. Speak with your doctor if you wish to try probiotics for constipation.
5. Lower Stress with Mindfulness Meditation
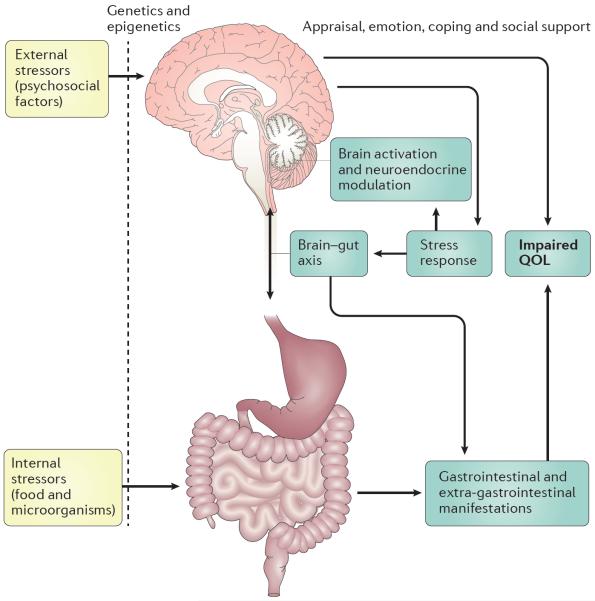
The brain and the digestive tract are so closely linked that researchers have coined the term ‘gut-brain axis’.
Digestive symptoms like constipation can lead to anxiety and psychological stress. In turn, stress strongly affects the gut.
Chronic stress is known to modify the gut microbiota and to alter nerve action in the intestines (18).
Psychological stress influences the gut both directly and indirectly. Availability of coping mechanisms and social support helps determine severity of symptoms and impact on quality of life. Click to enlarge. Image source.
It’s important to manage stress, both for overall health and to ease digestive symptoms.
Mindfulness meditation has shown particular promise in reducing IBS symptoms (19, 20).
In one high-quality study, IBS patients who received online mindfulness training reported a 42% reduction in symptoms at 3 months. By contrast, IBS patients who had access to an online discussion forum reported a 12% increase in symptoms (21).
The study also showed that the benefits of mindfulness training appear to be long-lasting. Participants who completed all mindfulness training sessions reported sustained benefits 15–18 months after the study ended, even without seeking additional treatment (22).
The cell phone app Headspace offers a free trial of guided mindfulness meditation sessions. There are also many resources online that teach how to practice mindfulness.
Summary: Interactions between the gut and the brain cause stress to aggravate IBS symptoms, including constipation. Studies have shown mindfulness meditation can help relieve symptoms.
6. Move Your Body

Physical activity is often recommended by medical professionals to help ease chronic constipation.
It’s said to to shorten intestinal transit time, but research on physical activity and constipation is conflicting.
One observational study of older adults linked low physical activity levels to constipation. The study also looked at other factors, such as diet variety, that influence bowel symptoms. It’s difficult to know from this study the degree to which inactivity is related to constipation (23).
Other studies haven’t shown a strong link between exercise and constipation relief. One study even showed that intense exercise may worsen symptoms for some patients, while other studies have shown that exercise does not affect stool transit time (14, 24).
Even if exercise doesn’t directly improve constipation, it may still be helpful for those with the condition.
In one study of 140 adults with constipation, those who exercised more reported higher quality of life than those who were not as active (25).
Physical activity can also be very helpful in reducing stress, which is strongly linked to IBS symptoms.
Healthy adults should aim for at least 150 minutes of moderate-intensity exercise per week.
Summary: There is not enough evidence to show that exercise directly influences constipation risk or symptoms. However, exercise has been shown to improve quality of life in constipated patients, and it may help relieve stress.
7. Try Abdominal Massage

Abdominal massage has been used to treat chronic constipation since the 1800s.
Specific massage techniques help move stool through the intestines more quickly by increasing bowel muscle contraction (26).
Massaging the abdomen has shown particular promise in relieving constipation among those with certain medical conditions such as Parkinson’s disease and physical disability (27, 28).
It’s also been shown to improve quality of life for constipated patients.
In one study of 60 volunteers, abdominal massage plus laxatives improved health-related quality of life significantly more than laxatives alone (29).
Abdominal massage is considered safe for most and can be learned for free using online video tutorials. It can’t hurt to try it in conjunction with other diet and lifestyle changes (26).
Summary: Certain abdominal massage techniques can help move stool through the bowel. Massage is safe for most and can be performed at home.
8. Go When You Have To and Prop Up Your Feet

Certain practices before and during bowel movements can help reduce chronic constipation symptoms.
Bowel withholding is one common habit that may increase risk.
Occasionally resisting the urge to move the bowels is probably not harmful. Frequent withholding of stool, on the other hand, may cause the stool to dry out and become more difficult to pass.
Chronic stool withholding may lead to nerve damage and cause the bowel wall to become stretched. These issues could, in turn, worsen constipation (30).
It’s best to move the bowels when you have the urge.
Certain body positions may make it easier to fully evacuate stool. Studies have shown that a semi-squatting position, with the feet slightly elevated (hips about 35-degree angle), results in significantly less retained stool in the colon (31, 32).
Squatting is believed to help by widening the anorectal angle and lengthening the pelvic floor muscles, which allows for easier passage of stool (32).
Summary: Moving the bowels when the urge first strikes and slightly elevating the feet when defecating may reduce risk of constipation and minimize straining during bowel movements.
9. Over-the-Counter Treatments for Constipation

Diet and lifestyle changes should be the first steps in treating constipation.
Occasionally, over-the-counter laxatives may be useful for constipation that causes significant discomfort or that does not resolve with gentler measures.
There are 4 main types of over-the-counter laxatives:
- Bulk-forming laxatives (e.g., Metamucil) increase the size of stool while also softening it.
- Surfactant or softening laxatives (e.g., Colace) soften the stool by drawing water and fats into it.
- Osmotic laxatives (e.g., Miralax) help the bowel to hold more water, which helps stool move through the bowel more quickly.
- Stimulant laxatives (e.g., Senna) trigger the nerves in the colon to increase contractions.
It’s very important to speak with a doctor before beginning any constipation treatment, due to the risk of side effects.
For example, bulk-forming laxatives are not recommended for many older adults, who tend to drink less fluids. Those with heart and kidney problems should not use osmotic laxatives due to risk of fluid and electrolyte imbalances (33).
Lastly, note that excessive use of laxatives can worsen constipation, which is why it’s not a long-term solution (34).
Summary: Laxatives should not be a first line treatment for constipation. It’s important to speak with a doctor before using them and to use them sparingly to avoid dependence.
10. Certain Supplements May Help
Anecdotal evidence and small studies suggest that certain supplements may ease constipation symptoms.
Most of these remedies have not been shown to be effective or safe.
Fig Paste (Ficus carica)
Fig paste is available in stores or can be made at home.
Human and animal studies have found it to be effective in reducing colon transit time and improving stool output and consistency. Human studies have also shown it to reduce abdominal discomfort (35, 36).
In one human study, the effective dose was 300 grams per day of fig paste containing 1.7% fiber for 4 weeks. This is generally regarded as safe for otherwise healthy adults (35).
However, those who are sensitive to FODMAPs may need to avoid figs due to their high fructose content.
Aloe

Aloe is a plant that grows throughout the world.
Aloe gel is taken from deep within the leaves and commonly applied to the skin to relieve sunburn and other minor irritations.
Aloe latex is found just under the plant’s surface and is reported to be a strong laxative when taken orally.
One small study from the 1970s found aloe latex to be more effective than the stimulant laxative phenolphthalein in relieving constipation (37).
Unfortunately, it may not be safe to take orally. In fact, the FDA reports that ingestion of aloe latex may increase risk for cancer and cause interactions with prescription drugs.
Mineral Oil
Mineral oil has long been said to ease constipation by lubricating the stool.
However, long-term use of mineral oil has been linked to significant health risks, including vitamin malabsorption and aspiration pneumonia (38, 39).
Speak with your doctor before treating constipation with mineral oil.
Summary: Fig paste may be helpful for treating constipation and is likely safe, although high in FODMAPs. Aloe latex and mineral oil are not recommended due to possible side effects and drug interactions.
When to Call Your Doctor

Constipation can often be treated at home, but chronic constipation that interferes with quality of life warrants a visit to the doctor.
Unresolved chronic constipation can result in fecal impaction. With impaction, the bowels cannot be evacuated just by the normal muscle contractions that push stool out of the body. Medical intervention is usually needed.
Speak with your doctor if (10, 14):
- You have a fever, rectal bleeding or recent weight loss.
- Your symptoms interfere with sleep.
- You are frequently constipated and have a family history of bowel disease.
- You can feel a lump or mass in your abdomen or rectum.
- You are over 50 years old and chronic constipation is a new problem for you.
- You have severe abdominal pain and vomiting.
- You are not passing gas.
The Punch Line
Chronic constipation is a common problem that most of us will experience at some point.
To a large degree, treatment must be individualized based on tolerance for diet and lifestyle changes.
Still, certain approaches are backed by science:
- A trial of a low-FODMAP diet can help identify food sensitivities that worsen constipation.
- Gradually increasing soluble fiber, either through diet sources or psyllium supplements, has shown some benefit.
- Avoiding dehydration can help prevent constipation.
- Stress management is key. Mindfulness meditation has shown great promise. Exercise and other stress-reduction methods are useful as well.
- The probiotic lactis has been shown to improve bowel transit time and IBS symptoms.
- Abdominal massage, posture changes during bowel movements, and evacuating when the urge first strikes are safe for most and may help with regularity.
- Laxatives may be used as a last resort.
Always speak with a doctor before starting a new supplement or medication, or if you have any symptoms that are alarming.
Would you like more information on how to start a low FODMAP diet?
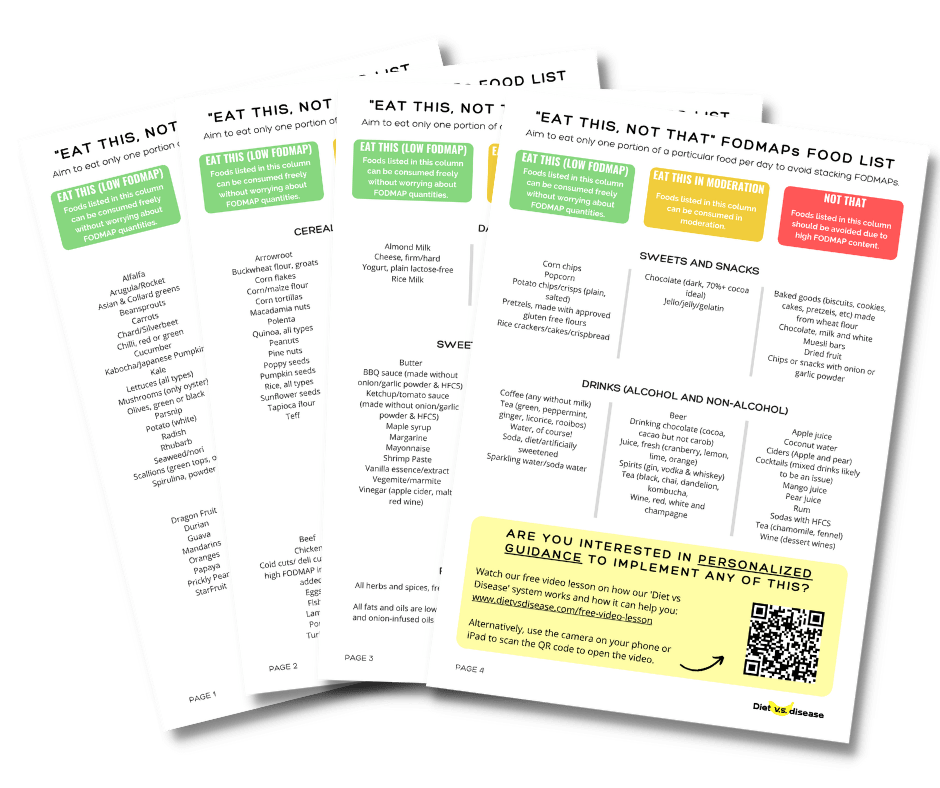
Tap the blue button below to download our “Eat This, Not That” list as well as additional resources for IBS and digestive issues (it’s free!)