[Last updated 7th March, 2023]
Any sort of abdominal pain can be frustrating.
Add bloody stool to the mix, and it can turn downright scary.
Often these types of symptoms are linked to an issue in the gut, and they may be tricky to diagnose and ultimately treat.
Ischemic colitis is one of these conditions, and it’s often confused with other inflammatory bowel diseases.
This article clears up any confusion about what ischemic colitis is and the best short- and long-term treatments and dietary plans to keep symptoms at bay.
What is Ischemic Colitis?

Ischemic colitis (IC) is an inflammation of the large intestine (colon) that is caused by a lack of blood flow to the colon.
Ischemia refers to an inadequate blood supply to an organ, in this case the colon.
It’s typically broken down into two forms:
- Non-Occlusive Disease: This is the most common type of IC and involves decreased blood to the colon, not due to a blockage. There are various reasons this may happen, including decreased blood pressure caused by a heart condition or a reaction to medication taken for lowering blood pressure.
- Occlusive Disease: This is caused from the blockage of an artery or vein that supplies blood from the aorta (the main artery of the body) to the colon.
Aside from the inflammation, this condition is not related to other inflammatory bowel diseases (IBD) like ulcerative colitis or Crohn’s disease , microscopic colitis , or similar conditions like pseudomembranous colitis (C. diff colitis).
Most often symptoms are short-term, but about 20% of patients will develop chronic IC that may require surgery (1).
Acute ischemic colitis involves sudden and serious abdominal pain; in this case, immediate medical attention and surgery is necessary.
Ischemic Colitis vs. Mesenteric Ischemia
Though symptoms are similar, ischemic colitis is not the same as mesenteric ischemia.
Here are the prime differences:
Ischemic colitis:
- Involves lack of blood to the colon.
- Typically characterized by lower abdominal pain and tenderness, as well as bloody stools and diarrhea.
- Symptoms are usually short-term and surgery is often not necessary.
Mesenteric ischemia:
- Involves lack of blood to the small intestine.
- Typically characterized by abdominal pain experienced about 2 hours after eating, as well as weight loss, nausea, vomiting and occasional bloody stool.
- In cases of acute mesenteric ischemia, severe abdominal pain is experienced and immediate care is necessary, often in the form of surgery.
Summary: Ischemic colitis (IC) is an inflammation of the large intestine (colon) caused by restricted blood flow to the colon. This may be due to decreased blood pressure or a blockage of an artery or vein. This form of colitis is not related to ulcerative, microscopic or C diff. colitis. It’s also less serious than mesenteric ischemia, which involves a lack of blood supply to the small intestine.
Ischemic Colitis Symptoms, Causes and Diagnosis

Since its symptoms resemble other inflammatory bowel diseases (IBDs) and gastrointestinal issues like diverticulitis, IC can sometimes be misdiagnosed.
To rule out other conditions, a number of tests may be recommended including stool analysis, ultrasound and abdominal CT scans, CT or MRI angiography (to look at arteries and blood flow) and colonoscopy.
IC Causes & Risk Factors
IC most often occurs in people over 60 years old. Most diagnosed with it are also facing other underlying illnesses including:
- Atherosclerosis (plaque buildup in arteries)
- Pre-diabetes and diabetes
- Very low blood pressure (often due to heart failure, surgery or severe trauma)
- Past history of surgery involving the abdominal, heart, aorta or blood vessels
- Irritable bowel syndrome (IBS)
- Chronic constipation
- Blood clots
Those who smoke, use cocaine or methamphetamines, or take certain medications—like antibiotics or those that cause constipation—may also be at greater risk (2).
IC can also occur in endurance athletes like marathon runners and triathletes. Staying well-hydrated with plenty of fluids and electrolytes is crucial for prevention of an IC attack during intense bouts of exercise (3).
It has even be linked to the herbal weight loss supplement known as ma huang or ephedra, which has long been banned by the U.S. Food and Drug Administration for its adverse side effects. However, ephedra extracts are still legal (4).
Ischemic Colitis Symptoms
The most common symptom of IC involves abdominal pain and cramping, often on the left side of the abdomen.
You may also experience:
- Loose and bloody stools, and sometimes only blood with no stool (if bleeding occurs in excessive amounts, it may be another condition like Crohn’s or colon cancer)
- Tenderness in abdomen
- Urgent need to have a bowel movement
- Diarrhea
- Vomiting
If you’re experiencing severe and sudden pain on the right side of your abdomen, this could indicate a more serious problem that may also involve blockage to your small intestine.
If this is the case, seek medical care immediately; you may require emergency surgery.
In most cases, however, symptoms should cease within two to three days.
Summary: IC most often occurs in people over 60 years old, particularly those with underlying conditions like atherosclerosis, low blood pressure, IBS, blood clots or diabetes. The most common symptoms include abdominal pain and cramping and loose and bloody stools. Symptoms should typically go away within a few days.
Treatment for Ischemic Colitis

Treatment for IC typically includes a round of antibiotics, IV fluids and a liquid diet.
After diagnosis, most patients will be prescribed antibiotics to prevent infection, and will likely be encouraged to avoid any medications that reduce blood flow.
They may also be given intravenous (IV) fluids to help with hydration, and be placed on bowel rest to give the digestive tract a necessary break.
A clear liquid diet may be recommended—more details on this below.
For mild IC, some people may not even require any medical attention, but in severe cases, surgery is necessary if the lack of blood flow leads to tissue death in the colon. This dead tissue will need to be removed immediately to avoid further complications.
Summary: Typical treatment includes antibiotics, IV fluids and bowel rest with a clear liquid diet. Mild cases of IC may not even require any medical attention, while severe attacks could necessitate emergency surgery.
Ischemic Colitis and Diet Recommendations

Diet does not directly cause IC, but it can certainly help manage it as well as any underlying conditions.
As mentioned above, a clear liquid diet is often recommended immediately after an IC episode. This includes:
- Water
- Clear juices like apple, white grape or cranberry juice (without pulp)
- Broth
- Black coffee or tea
- Plain gelatin
- Sodas and carbonated beverages
- Popsicles (without pieces of fruit, pulp or yogurt)
These liquids are easy to digest and provide electrolytes for optimal hydration. Since this diet is highly restrictive, it should only be followed for no more than a few days.
As you start to add foods back in, continue to keep things easy on your digestive system. Here are a few tips:
- Gradually increase your fiber.
- Stay hydrated; aim for at least 64 oz. per day.
- Eat smaller, more frequent meals instead of a few large ones.
- Chew your food thoroughly to help break it down.
Long-Term Diet Plan for IC Prevention
There’s no set diet specifically for ischemic colitis.
In fact, it’s best to address any underlying condition that may have caused IC with a well-balanced whole foods diet that minimizes inflammation.
Some recommend trying a low-residue diet, which limits high-fiber foods like whole grains, fruits and vegetables, and nuts and seeds that can leave undigested “residue” in the stool.
People with Crohn’s disease have found some relief on this type of diet, so it may extend to helping those with IC.
That said, no research has been shown to prove the effectiveness of the low-residue diet. In fact, eating more fiber may actually be far more beneficial (5).
Foods to Eat:
You’ll want to focus on foods that are anti-inflammatory, can help maintain a stable blood pressure, and boost HDL (good cholesterol) levels to keep your arteries and veins healthy.
Along with fatty fish (like salmon and sardines) and nuts and seeds, you’ll want to consume plenty of fresh fruit and vegetables. If you have trouble digesting them raw, choose softer fruits (like bananas) and well-cooked vegetables.
In particular, watermelon is a good source of citrulline, an amino acid that helps with blood circulation, including that within your digestive system.
No research has yet focused specifically on ischemic colitis and probiotics or anti-inflammatory herbs and supplements like curcumin, ginger and omega-3 fatty acids.
Foods to Avoid:
Overall, it’s best to avoid foods that may trigger inflammation in the gut including:
- Fried and fatty foods
- Spicy foods
- Sugary foods and beverages (including artificial sweeteners)
- Caffeine (coffee, tea, sodas)
- Alcohol
You may also want to try avoiding gluten and possibly lactose (found in dairy).
Some lifestyle changes may also be necessary. If you’re a smoker, you should quit immediately. Smoking raises blood pressure and causes plaque buildup in the arteries.
You will also want to talk to your doctor about switching out any medications that may have contributed to your IC, especially those that reduce blood flow or cause constipation.
Summary: No specific diet has been proven effective to prevent IC, but you will want to focus on eating foods that are anti-inflammatory, can help maintain a stable blood pressure, and boost HDL (good cholesterol) levels to control any underlying conditions. Avoid fried, fatty and spicy foods, alcohol and caffeine, and possibly gluten and lactose. If you smoke, quit immediately.
Is Ischemic Colitis Manageable?
Fortunately, IC is most often a temporary condition that can resolve within a few days.
Unlike other forms of inflammatory bowel disease or colitis, IC is typically short-term. It can, however, turn into a chronic problem if a buildup of plaque in the arteries (atherosclerosis) worsens.
Most often, a clear liquid diet and antibiotics are prescribed immediately after an IC attack to help heal the digestive system and protect your colon from infection.
Overall, your main goal is to focus on any underlying condition (or medication) that may be restricting blood flow to your colon, including cardiovascular disease, atherosclerosis, blood clots, low or high blood pressure or diabetes.
Of course, eating a well-balanced diet of fresh, whole foods is one of the surest ways to improve all of these conditions and ultimately prevent IC for good.
Would you like more information on how to start a low FODMAP diet, which can help with many forms of colitis?
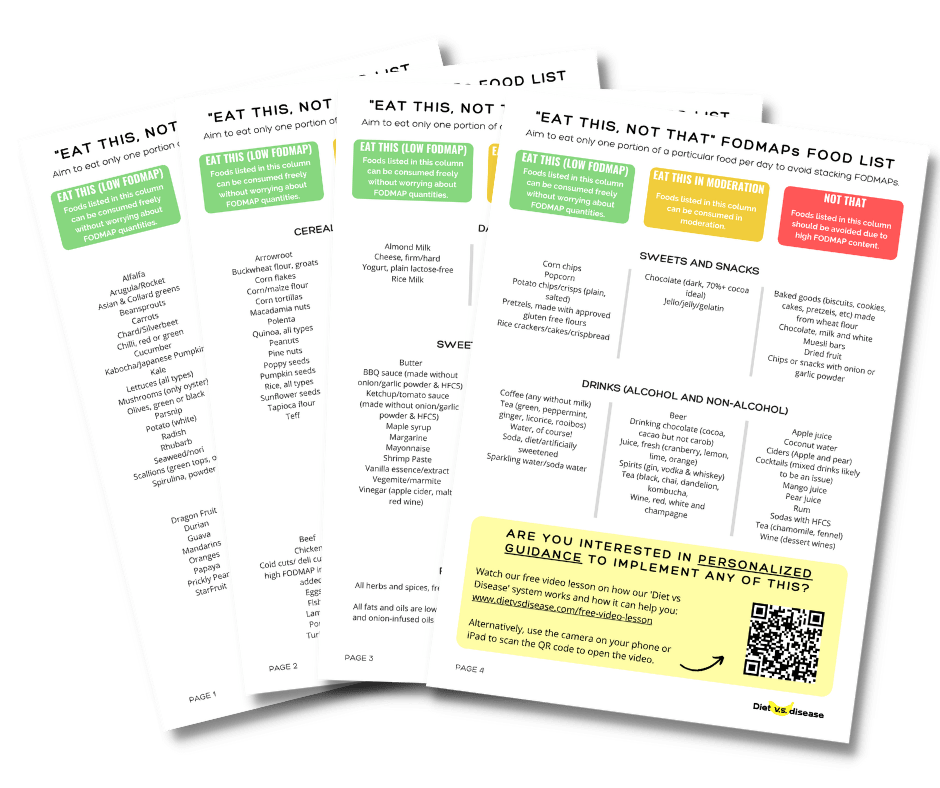
Tap the blue button below to download our “Eat This, Not That” list as well as additional resources for IBS and digestive issues (it’s free!)
