So you’ve experienced just how awful a diverticulitis flare-up can be.
Or perhaps you’ve had multiple flare-ups and you don’t want to go through that anymore.
The good news is based on my experience of more than 10 years in the field, I’m going to share with you two fundamental steps that will ensure that you get symptom-free and that you restore your gut health and resilience.
And so you know, I’m not going to tell you to increase your fiber. In fact that guidance is wrong and I’ll explain why in this article. So if you’ve been told to increase your fiber, then this article is especially for you.
The Importance of Managing Flare-Ups
Before we go to step 1, I think this section is very important.
And I don’t want to scare you, I just feel like this never gets spoken about enough.
The reality is if you do not figure out how to manage your flare-ups, they do increasingly more damage to your intestines.
At some point if you keep having flare-ups your GI doctor is going to have a stern conversation with you about surgical procedures to treat diverticulitis, so it’s really important you do everything you can to get this under control.
Summary: Manage your diverticulitis flare-ups to avoid damaging your intestines and to reduce your risk of requiring surgery.
Step 1: Discover What Foods You Do And Do Not Tolerate And Why

I want to tell you a quick story that really emphasizes this first step.
It’s about a client of ours named Beth who had diverticulitis for more than 10 years.
Beth was a registered nurse for 30+ years and she thought that she could get a lot of the answers and information about diverticulitis herself.
However, the problem was in the past year she’d had multiple trips to the ER, hospitalizations and too many flare-ups, so the doctors wanted to take out the sigmoid portion of her large intestine. This would require her to live with a colostomy bag.
So of course Beth wanted to try to manage things herself. She had previously tried nutritionists and dietitians, but they had given her some food lists or meal plans that just weren’t very useful and she wasn’t getting anywhere.
When Beth found us we were able to help her identify what exact foods were triggering issues and then help formulate an eating pattern where she could still enjoy her favorite foods, eat with freedom and go out without having to worry about having a diverticulitis flare-up.
So long story short, Beth got her gut issues under control and she didn’t have to have that surgery.
How To Discover What Foods You Do And Do Not Tolerate

If you have lots of bloating, irregular bowel habits and gut issues regularly, then you need to get that sorted out as well.
Even though they may or may not be directly triggering diverticulitis flare-ups, they’re certainly not helping with the inflammation and the pain that you’re experiencing.
It’s like if you had a really bad burn on your arm and then you constantly put vinegar on it and alcohol and scrubbed it. It would be very painful and irritated and it would never get better.
The same can be said for your digestive tract, specifically the intestines and that’s what’s going on when you have diverticular disease.
So the way we discover what foods you do and do not tolerate is by following an elimination protocol – typically a low FODMAP diet – which is a temporary eating pattern that removes certain compounds and then strategically reintroduces or rechallenges them back into your diet.
This way you can actually pinpoint what food compound was triggering symptoms and in what quantity.
This is a key step to be able to introduce more foods back into your diet and not feel worried or anxious about whether a food is going to trigger my symptoms or not.
Low FODMAP Diet For Diverticulitis

This part is dependent on the person, but we’d usually start you on a low FODMAP diet, which is the most well-studied diet protocol for digestive issues and appears to help with diverticulitis as well.
To do it on your own essentially you want to track down what you’re eating and then record your symptoms. That way you can connect the dots.
Now you can write it down as a symptom diary, or for our clients we have an app that we use. The key is to be methodical and clear in your documenting, so think about it like a puzzle.
What’s the fastest and the most efficient way to solve a big giant puzzle?
First you would find the corners and the sides with the flat edges and you would put them together. Then you can start filling in from the outside in and it becomes much easier.
If you don’t have that structure and you have to build the puzzle from the inside out, it will take you forever to find the right pieces and to do it properly, so being methodical and tracking things down (i.e. like finding the edges and the corners of the puzzle).
The other thing that’s really important is that this is a short-term diet. We don’t do it forever. If you’re following a low FODMAP diet for years and years then you’re doing something wrong and you need to get some guidance there, because it’s a temporary protocol. It has a start and it has a finish.
Summary: Step 1 is about figuring out what foods trigger symptoms and inflammation for you personally. Typically this is done by following a low FODMAP diet, which has a start and an end. Being methodical about recording what you eat and the symptoms you experience, as well as reintroducing foods properly, will allow you to identify those food triggers and minimize flare-ups.
Would you like more information on how to eat for diverticulitis?
Tap the blue button below to download our “Eat This, Not That” list as well as additional resources for diverticular disease (it’s free!)
Step 2: Get Clear On The Environmental And Lifestyle Factors Impacting Your Health

For this step let’s do a visualization exercise.
So I want you to imagine you’re hanging out by a river and you see someone drifting past in the river. It’s quite fast and they’re drowning, they’re struggling and calling for help.
In this scenario you’re a really strong swimmer, so you jump in and you save them. You grab them and you paddle back into shore.
So now you’re catching your breath and then another person comes past and needs help, so you jump in and you go and save them too.
This one was much more of a struggle, because you’re getting tired now. You’re really exhausted and you’re getting worried…what if there are more people?
If someone else comes past you might not be able to help them, so you decide to start running up stream to see where these people are coming from.
You finally come across a small bridge and sure enough there is a well-concealed hole, and that’s where people are falling through.
So you fix the hole and you put up a sign to warn people so that nobody falls in anymore.
And that’s the punch line here.
Oftentimes we’re so concerned with the immediate problem, like people floating downstream, or in this instance your diverticulitis flare-ups as they occur, that we don’t go upstream and figure out what is causing the problem, or what is the root cause of the flare-ups.
With the diverticulitis you’re experiencing, we know it’s not solely one food you ate or one thing you did that caused it, otherwise treating it would be so simple. But it’s not.
That’s why when you look online you get conflicting information everywhere and it’s very unclear…
Which is why step 2 is to get a clear road map of the environmental and lifestyle factors that influence your health.
In other words, what are the factors that contribute to diverticulitis and are we ticking those boxes to make sure they don’t apply to us.
What Factors Do We Need To Consider?
Take a look at this diagram from the World Journal of Gastrointestinal Surgery.
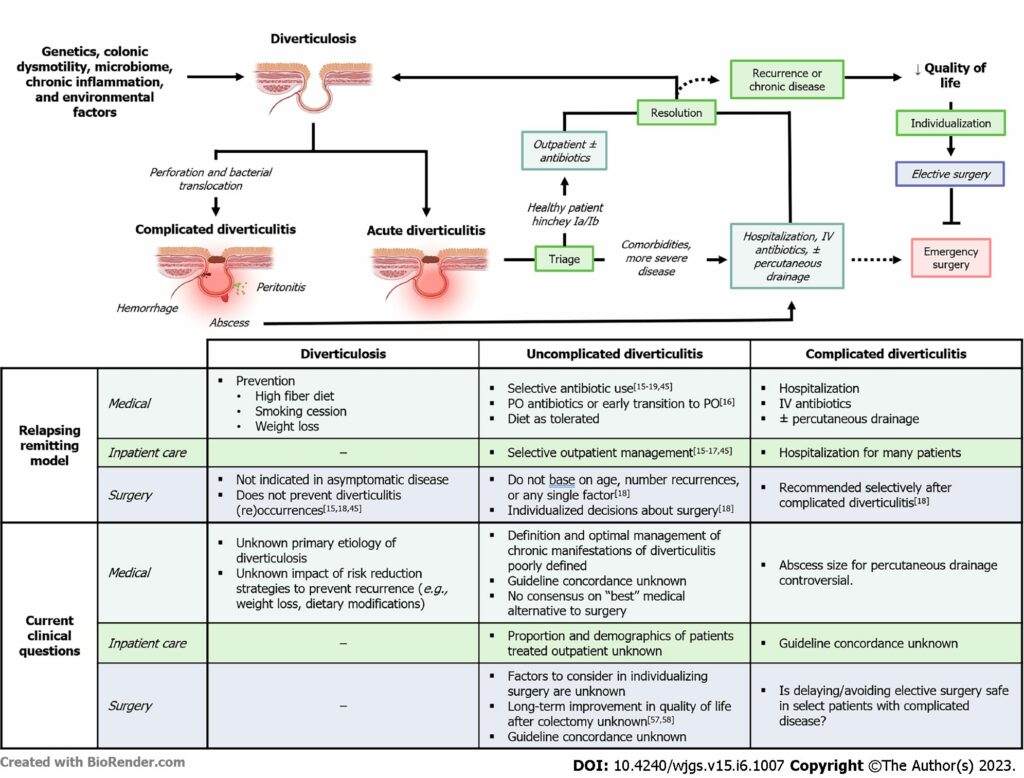
Specifically, look at the top left section. The researchers now understand that contributing factors to diverticulitis are:
- Genetics
- Colonic dismotility
- Microbiome
- Chronic inflammation, and
- Environmental factors.
First of all, do you know what stands out to me the most? It doesn’t say anything about fiber there, and I’m going to explain that more at the end of this article.
So granted genetics is one factor that’s not in our control, right? But that is not how you should think about it.
I heard a quote when I was studying nutrition that’s always stuck with me. It says “your genetics loads the gun, but it’s your environment and lifestyle that actually pulls the trigger.”
In other words, just because a condition runs in your family, it’s not a death sentence. In fact, you have the ability to delay when the onset occurs or from it even occurring at all.
For example, for me prostate cancer runs in my family at every generation, so it’s a huge worry for me. It’s very likely that I will get it, but I can quite possibly delay its onset for many decades or perhaps even prevent it from occurring ever.
It depends on my lifestyle and environment.
So back to diverticulitis… Ask yourself:
- Am I a healthy weight?
- Do I have a lot of visceral fat around my organs and gut?
- Do I meet my protein intake every day?
- Is my heart health good?
- Do I take cholesterol medications?
- Am I on blood pressure medications?
- Do I regularly consume foods that I don’t tolerate well, but I do it anyway and how does that affect my gut microbiome?
- Are my bowel habits typically healthy or not?
- Is my environment or lifestyle super stressful or high anxiety?
- Do I have chronic inflammation?
I could go on and on, but you get the idea.
If your answers are typically not what they should be, then it’s time to get serious about making some meaningful changes in your life.
And yes, I know it can feel overwhelming…where do you even start? How do you make time for these things and how do you stay committed to changes once you’ve started to make them?
It’s not easy, but it is simple and the good news is I have the answers for those questions. I can touch on it at the end of this article.
Summary: Step two is to get a clear road map of the environmental and lifestyle factors that impact your health so that you can make meaningful, sustainable changes where you need to.
What About Fiber Intake?
Not all fiber is equal.
There’s many different types of fiber and many different food sources of fiber too.
The problem is foods that are high in fiber are typically high in FODMAPs as well. So if you’re sensitive and you increase your fiber, you increase your FODMAP exposure and guess what happens? You get more symptoms.
Because of this the blanket advice from your doctor to increase your fiber intake to prevent flare-ups is wrong, as almost all of the time that recommendation doesn’t have any context about you.
It’s like if I asked you, how long is a piece of string?
To answer that correctly would depend on what string you have and what it looks like, right?
It’s actually impossible to answer that question without more context and so it’s the same with this fiber recommendation people have given.
You can’t give it without more context, without knowing what the patient is sensitive to, what is their medical history, what are their eating patterns like, etc.
Summary: High fiber foods are typically high in FODMAPs as well, so if you increase your fiber you may experience more gastrointestinal symptoms. Increasing your fiber intake, as well as with which type of fiber, needs to be personalized to you.
Treating Diverticulitis Is Simple, But Not Easy
Step one to treating diverticulitis is to discover what foods you do and do not tolerate and why. Often a low FODMAP diet can help identify your food triggers and reduce inflammation.
Step two is to get a clear road map of the environmental and lifestyle factors impacting your health. Determine if you are ticking all the right boxes or what areas you are lacking in.
The other consideration is fiber, in that you do not always need to increase your fiber, and it also depends on what type of fiber you are having. This differs from person to person and needs to be approached in a more methodical way than most are doing.
Ultimately, if you follow these instructions then managing diverticulitis can be a simple process…
But that does not mean it’s an easy process because you need to be consistent with the changes you make. That’s often the hard part.
If you want to learn more about how we might be able to help you, I invite you to apply for a nutrition assessment call with us.
Diverticulitis and related digestive disorders is what we specialize in, and we are the world’s leading team to do this online.
