Endometriosis is a painful condition that can greatly impact your quality of life.
Diet changes are said to help relieve symptoms, but does the evidence support these claims?
This article explores the role of diet in endometriosis treatment.
What is Endometriosis?
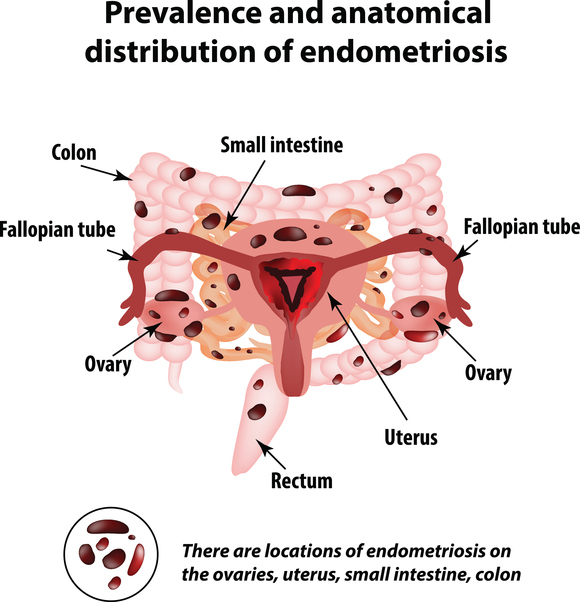
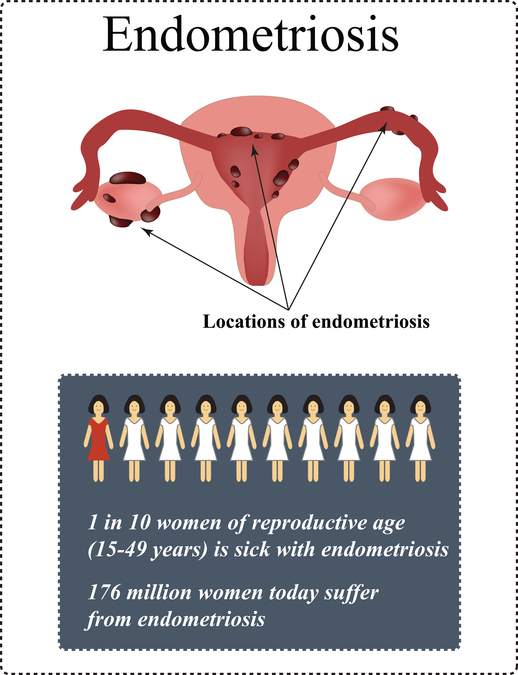
Endometriosis occurs when tissue that’s normally found inside the uterus grows in other parts of the body.
Endometrial tissues normally build up in the uterine lining each month until the lining is shed during the menstrual period.
For various reasons, these cells are found in other parts of the body in women with endometriosis, causing inflammation and scarring at affected sites.
Click to enlarge.
Tissue deposits (called implants) are most often found in the pelvis, but can also be found in more distant organs like the liver and the brain (1, 2).
Endometriosis Symptoms
Some women with endometriosis have no symptoms.
In fact, it’s often discovered during medical tests or surgeries for other conditions (3).
However, most women experience symptoms that significantly affect quality of life, including:
- Pelvic or lower back pain
- Painful menstrual periods (dysmenorrhea)
- Heavy menstrual periods
- Pain during intercourse
- Painful bowel movements or urination
- Fatigue
- Bloating
- Digestive Distress (constipation, diarrhea, or nausea)
The condition affects up to 10% of women. It’s typically seen in women of childbearing age, but symptoms may persist into menopause or after hysterectomy if estrogen levels are high enough (4, 5).
Up to half of affected women also struggle with infertility, but it’s not known whether endometriosis causes infertility or is just associated with it (6, 7).
Interestingly, cases of endometriosis have also been reported in men, but this is incredibly rare. It’s most common in men who’ve received estrogen therapy to treat prostate cancer (8).
Summary: Endometriosis affects up to 10% of women and causes tissue that’s normally found in the uterus to build up in other parts of the body. Symptoms include pain, heavy menstruation, digestive distress, fatigue, and bloating.
Endometriosis Causes

Endometriosis is thought to be caused by a combination of genetic, physiologic, immune, and environmental factors (9).
In fact, studies have found that a woman’s risk increases by up to 7 times if her mother or sister has it (10).
However, not everyone with a family history will develop the disease. Other factors appear to increase the likelihood of endometriosis.
One of the most common theories is retrograde menstruation, which occurs when endometrial cells and menstrual blood travel upward via the fallopian tubes. From there, the cells can implant into the abdominal lining and onto the organs, causing inflammation and scarring (11).
Nearly all women experience some degree of retrograde menstruation, but it’s been suggested that a higher volume of blood enters the abdomen in women with endometriosis (12).
Two other common theories include:
- Coelomic metaplasia, which occurs cells in the abdominal lining mutate into endometrial implants through a series of reactions in the body. Similarly, it’s been proposed that stem cells and bone marrow cells might change into endometrial implants (6, 13).
- Lymphovascular trafficking, which is the spread of endometrial implants through the lymphatic system.
However, these are just theories for now, and it seems other factors likely play a role as well.
Oxidative stress appears to be a key one. It’s a term that describes cellular damage from molecules called free radicals.
Oxidative stress can be caused by exposure to chemicals and pollutants, stress, and other stimuli including the process of ageing itself (14).
Is Endometriosis an Autoimmune Disease?
Recent research also suggests the immune system could greatly influence disease onset and severity.
Autoimmune disease develops when the body’s immune system mistakenly attacks healthy tissues.
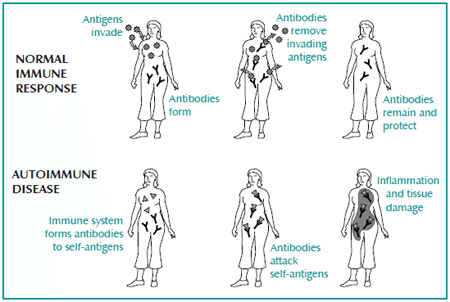
Image source: womensinternational.com
Endometriosis shares several key features with autoimmune disease, including systemic inflammation and the presence of autoantibodies. There’s also a strong overlap between endometriosis and other autoimmune conditions, like celiac disease and Graves’ disease (15, 16, 17, 18).
These similarities have many experts asking whether endometriosis should be classified as an autoimmune disease instead. It’s an emerging area of research that will likely be explored in greater depth in coming years.
Summary: Endometriosis is likely caused by a combination of genetic, immunological, physiological, and environmental risk factors. It’s similar in many ways to autoimmune disease, although it’s not considered to be one at this time.
Diet and Endometriosis

There’s no known cure for endometriosis.
The condition is commonly treated with surgery, hormone therapy, and medications.
No diet has been proven to treat endometriosis either. However, small studies and patient reports suggest that certain diet strategies can help reduce disease risk and lessen symptoms.
This could be because certain foods can help control inflammation and influence levels of certain hormones (estrogen and prostaglandins).
These include omega-3 fats, vegetables, and other foods, which will be discussed below.
Replace Trans Fats with Omega-3 Fatty Acids
Significant research has looked at whether fat consumption affects endometriosis risk and symptoms.
Unfortunately, some studies have found high-fat diets to be more beneficial, while others have found low-fat diets to be better (19, 20).
It’s a tricky area for researchers because fat quality is likely just as important as quantity, perhaps even more so (21).
Omega-3 fatty acids appear to be especially beneficial, while trans fats are thought to increase risk. In one study of nearly 71,000 women (21):
- Women who ate the most trans fats were 48% more likely to have endometriosis than women who ate the least.
- Women who ate the most fats from animal products—and especially palmitic acid—had a 20% higher prevalence of endometriosis than those who ate the least.
- Women who ate the most omega-3 fatty acids were 22% less likely to have endometriosis than those who ate the least.
Even modest increases in omega-3 fat intake appear to be beneficial. One study found that replacing 1% of calories from trans fats with omega-3 fats decreases risk by 50% (21).
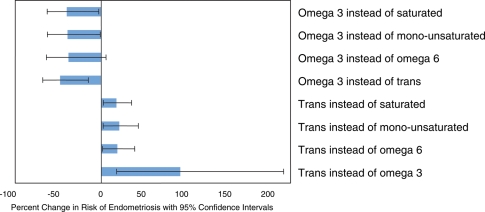
Changes in endometriosis risk seen when 1% of calories from monounsaturated, omega-6, trans, and saturated fats are replaced with omega-3 fats (top bars). Bars that extend further to the left represent larger reductions in disease risk. Image Source
The exact mechanism for this is unknown, but omega-3 fats have been shown to reduce inflammatory chemicals in the body, including cytokines and certain types of prostaglandins (22, 23, 24, 25).
For the record, trans fats are bad for you in many ways so replacing them with omega-3s makes sense regardless of whether you have endometriosis.
Aim to eat at least 7 ounces (about 200 grams) of fatty fish per week, and limit baked goods, fried foods, and packaged items.
Summary: Studies suggest that a diet higher in omega-3 fats and lower in trans fats may reduce endometriosis risk and severity. The recommendation for healthy adults of at least 7 ounces (about 200 grams) of fatty fish per week would also be beneficial for women with endometriosis.
Identify Food Intolerance and Eliminate Trigger Foods

Food intolerance can cause unpleasant reactions to specific foods.
Common symptoms include digestive distress and skin rashes.
Small studies have found higher rates of food intolerance in women with endometriosis compared to healthy controls (26).
Troublesome foods vary widely from person to person, but these are the most common:
Gluten and Celiac Disease
Patient testimonials (reports) suggest that a gluten-free diet is effective in treating endometriosis.
This may be true, as some studies have shown an overlap between celiac disease and endometriosis.
This relationship isn’t fully understood, but it’s been proposed that chronic inflammation from celiac disease may trigger the onset of endometriosis (15, 27)
A gluten-free diet may even provide symptom relief for those who don’t have celiac disease.
In one study of 207 endometriosis patients, 75% of participants reported significant reductions in symptom severity after 12 months on a gluten-free diet. They also reported improved mental health, social function, vitality, physical function, and perceived healthiness after following the diet (28).
More studies are needed to understand the relationship between gluten and endometriosis. At the very least, those with celiac disease or a known sensitivity to gluten should strictly avoid it.
FODMAPs
FODMAPs are short-chain carbohydrates that are poorly digested in the small intestine.
They reach the colon largely intact and ferment in the gut, causing bloating, gas, abdominal pain, and other digestive symptoms for those who are intolerant of them.
Studies have established strong links between irritable bowel syndrome (IBS) and endometriosis (29).
A low FODMAP diet has been proven for treating IBS, and recent research suggests that it may be useful for easing endometriosis-related bowel symptoms as well. This is due in part to a high overlap rate between IBS and endometriosis.
In one study that included 58 women with both conditions, 72% of patients saw a great improvement in bowel symptoms after 4 weeks on a low FODMAP diet. The success rate for the low FODMAP diet was also significantly higher for women with endometriosis compared to women with just IBS (30).
Click here for more information on how to start a low FODMAP diet trial.
Autoimmune Protocol
Research has shown strong links between endometriosis and autoimmune disease.
The Autoimmune Protocol (AIP) is a strict elimination diet designed for those with autoimmune disease. It’s meant to correct imbalances in gut bacteria and reduce inflammation.
Unfortunately, there have been no scientific studies on it to date. But patients with various autoimmune diseases have reported symptom relief using the AIP in online forums.
Importantly, note that this diet is very restrictive. It’s meant to be a short-term fix to help identify food intolerances for those with diagnosed autoimmune diseases.
If you have severe endometriosis and another autoimmune condition, a trial of the AIP may help after discussion with your doctor.
A gentler, easier alternative would be to keep a food and symptom journal for several weeks to identify foods that trigger symptoms.
Summary: There’s a strong overlap between endometriosis and food intolerance. Gluten free or low FODMAP diets may be helpful in improving symptoms for some women. The autoimmune protocol may be helpful short-term for those who also have autoimmune disease.
Eat More Vegetables and Fiber

Everyone can benefit from eating more vegetables.
Among many other advantages, higher vegetable consumption is linked to lower risk of endometriosis.
One large study of 504 women found risk to be significantly lower in women who eat a lot of green leafy vegetables (31).
The mechanism for this isn’t fully understood, but many vegetables are high in antioxidants, which help combat oxidative stress.
Vegetables are also high in fiber, which has been said to help rid the body of excessive estrogen.
In one study of 242 women, those who had the highest dietary fiber intake had significantly lower levels of estrone and estradiol (both forms of estrogen) than women who had the lowest fiber intake. The exceptions in this study were grapefruit and avocados, which were linked to higher estrogen levels (32).
Surprisingly, evidence is more mixed when it comes to endometriosis and fruit consumption. One study found higher fruit intake to increase risk, while other studies have found women who eat more fruit to have lower risk (19, 31).
Aim for at least 5 servings of vegetables and 2 servings of fruit per day, endometriosis or not.
Summary: Vegetables contain antioxidants, which may help reverse oxidative stress that comes with endometriosis. Aim for at least 5 servings per day, including leafy greens. Evidence is less clear on fruit intake, but most women would likely benefit from a couple of servings per day.
Endometriosis and Soy

Phytoestrogens are estrogen-like chemicals found in plants.
Soybeans and soy products are the greatest dietary source, but phytoestrogens are also found in flax seeds, oats, fruits, herbs, and other foods.
A certain kind of phytoestrogen (called genistein) that’s found in soy products has been said to help convert testosterone into estrogen. Since endometriosis is estrogen-dependent, some have questioned whether soy should be avoided (34).
Few studies have directly examined the relationship between soy and endometriosis, but limited data indicate it’s neutral, and potentially even helpful.
In one study, women with higher concentrations of soy isoflavones in the urine were less likely to develop advanced endometriosis. This suggests that soy may help protect against the disease (35).
A 2017 study of 495 premenopausal women also found no link between a high soy intake or high urinary phytoestrogens and increased risk of endometriosis (33).
Based on the weight of evidence, soy products do not increase your risk.
Summary: Evidence is not conclusive, but it seems that a high soy intake has no impact on the risk of developing endometriosis. Likewise, it probably does not make endometriosis any worse.
Don’t Drink Too Much Alcohol

Moderate alcohol intake of up to 1 drink per day is generally considered safe for most women.
Beer, bourbon, and red wine contain phytoestrogens, which may convert to estrogen in the body. Just like soy, some have questioned whether they increase endometriosis risk (7, 36).
Three large studies have found risk to be higher among women who drink the most alcohol, while 3 other studies found no link between alcohol and endometriosis (31, 37, 38, 39, 40, 41).
Notably, an often-cited study found that a compound found in red wine called resveratrol may limit the growth of endometrial tissue. But the study was conducted on mice, who were given very high doses of the compound. It wouldn’t be possible to safely drink the amount of wine needed to see any benefit (42).
High alcohol intake causes many health problems, so it’s best to limit yourself to 1 drink per day at most.
Summary: Several studies have found endometriosis risk to be higher among women who drink excessive alcohol, but other studies haven’t shown a link. High alcohol intake, and especially binge drinking, has many negative health consequences. One drink or less per day is best.
Vitamins and Minerals for Endometriosis

Several vitamins and minerals have been reported to relieve symptoms common in endometriosis.
In many cases, studies on vitamins and minerals have used supplements rather than whole foods. As such, it’s difficult to know the amounts of food that would yield similar benefits.
Antioxidant Vitamins
Antioxidants are compounds that protect against oxidative stress and cell damage.
Studies suggest that oxidative stress contributes to endometriosis onset and severity. Research also shows that the antioxidant vitamins C and E may provide symptom relief (4, 9, 43)
In one study of 59 women with pelvic pain and either endometriosis or infertility:
- One group of 46 women received 1200 milligrams (mg) of vitamin E plus 1000 mg of vitamin C daily.
- A second group of 13 women received placebo (fake) pills daily.
After 8 weeks, the vitamin group had significantly lower levels of known inflammatory markers compared to placebo.
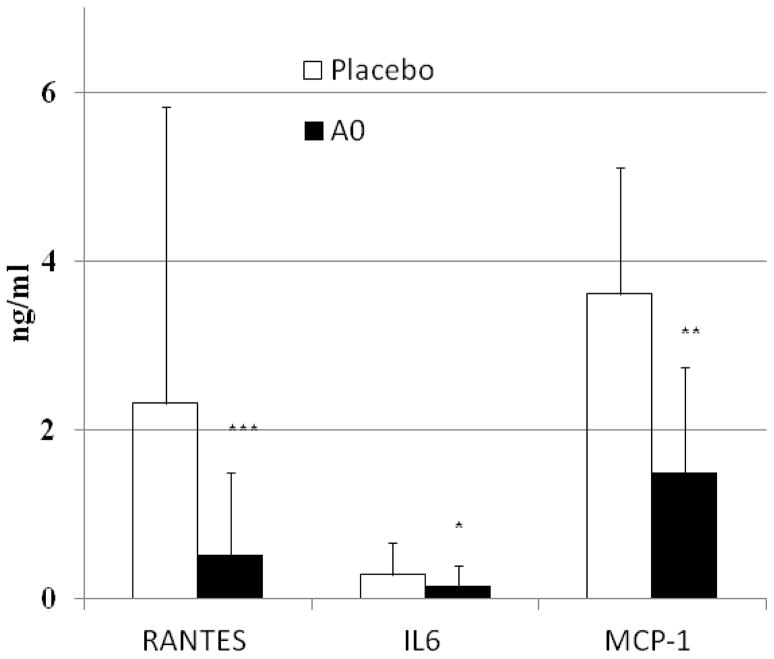
A comparison of inflammatory chemicals for the treatment and placebo groups. The black bars represent the treatment group, with a lower level being ideal. Image Source
Women in the vitamin group also showed significant reductions in self-reported everyday pain, compared to placebo (4).
Vitamin C is found in many fruits and vegetables and is particularly high in oranges. Vitamin E is found in foods like almonds and spinach.
Studies have also suggested that vitamin D may protect against endometriosis onset, although other studies have found it to have no significant effect on pain and other symptoms (44, 45).
Vitamin D is found in fortified foods, fatty fish, and egg yolks.
More human studies are needed to know the safest and most effective vitamin doses for endometriosis. Speak with your doctor before beginning any new vitamin or supplement.
Iron
Women with endometriosis may be at higher risk for iron-deficiency anemia due to heavy menstrual periods (46, 47).
Symptoms include fatigue, dizziness, headache, shortness of breath, pale skin, weakness, irregular heart beat, and cold hands and feet.
A simple blood test can help determine if you’re iron deficient. Your doctor may recommend supplements to help boost your iron levels.
Diet changes can also help to improve iron status for those who are anemic. Red meat is rich in iron, although it’s best not to consume fatty meats or large quantities of red meat (47).
Other diet sources of iron include seafood, nuts, green leafy vegetables, and fortified grain products.
For the record, the body absorbs iron from meat more effectively than from plant sources.
Thiamine
Vitamin B1 (thiamine) has been reported to ease menstrual pain.
One study of 556 young women with dysmenorrhea found that 100 mg of thiamine per day for 90 days completely relieved menstrual pain in 87% of volunteers and drastically reduced pain in 8% of volunteers (48).
Notably, this study didn’t include women with endometriosis, and thiamine was in capsule form. But it’s possible that it would help those with painful periods.
Know that thiamine deficiency isn’t common among healthy women in industrialized nations. More research is needed to know if higher dose supplements would affect endometriosis (49).
The Recommended Dietary Allowance (RDA) is 1.1 mg per day for women (who aren’t pregnant or lactating) and can be met by eating 3-5 servings of whole grains per day.
Magnesium
Magnesium is an element with many important functions in the body, including nerve and muscle regulation.
It’s available in many plant foods, including leafy greens, almonds, and beans. It’s also available in capsule, powder, and lotion form.
Three small studies have found magnesium to be more effective in reducing menstrual pain than placebo (50, 51, 52, 53).
Few adverse effects were reported in these studies, but supplemental magnesium may cause diarrhea, drowsiness, or other symptoms in some.
Magnesium deficiency is quite common, with nearly half of Americans consuming less than the RDA. Magnesium supplements can help ensure that daily needs are met (54).
Summary: Thiamine, magnesium, and vitamins C, D, and E have been reported to ease pain in endometriosis. Iron may be necessary for women with heavy periods. Ask your doctor if you might benefit from supplements.
Complementary and Alternative Treatments for Endometriosis
Several alternative therapies have shown some promising results for treating endometriosis.
Just note that much of the evidence so far is from preliminary and animal studies.
Probiotics
Probiotics are beneficial bacteria that are found in certain foods and supplements.
Recent research suggests that imbalances in gut bacteria may trigger or worsen endometriosis by altering estrogen and stem cell activity.
The bacteria Lactobacilli seems to play a key role in restoring a healthy balance. Studies of rhesus monkeys with endometriosis showed lower levels of these bacteria compared to healthy monkeys (55, 56).
One small study found the probiotic strain Lactobacillus gasseri to significantly reduce the total weight and surface area of endometrial implants in female mice.
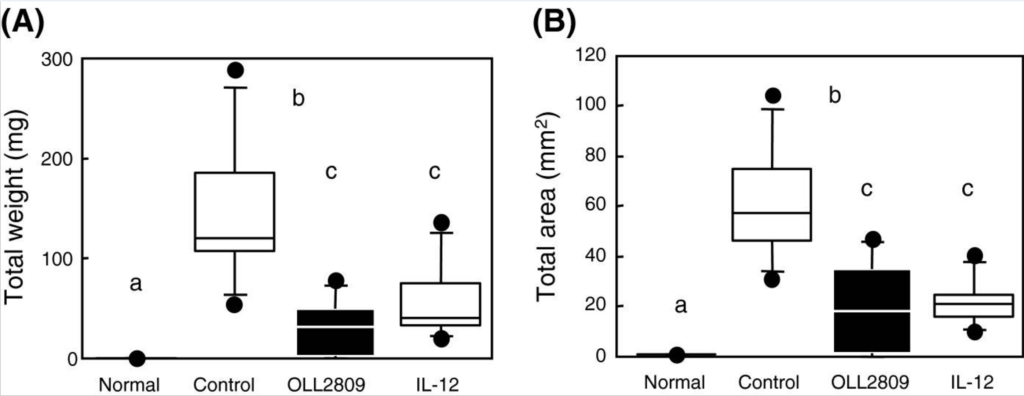
The effects of L. gasseri oral supplements on endometrial implant weight and surface area in female mice, compared to controls. A lower value is better. Click to enlarge. Image Source
The exact reason for this is unknown. Researchers believe that L. gasseri may increase levels of a cytokine called interleukin-12, which has been shown to reduce growth of endometrial tissue (56).
Human studies are needed to know the best probiotic strains and doses for endometriosis.
Melatonin
Melatonin is a hormone that’s commonly used as a sleep aid.
One small study has suggested that it may also help reduce the size of endometrial implants, at least in rodents.
One group of rats with induced endometriosis received injections of melatonin at a dose of 10 milligrams per kilogram of body weight every day for 4 weeks. The rats were then euthanized, and endometrial implants were measured.
Compared to controls (who were euthanized before melatonin treatment) rats who received the injections had significantly smaller and fewer implants (57).
Small human studies have also found melatonin to improve endometriosis symptoms, and particularly pain and use of pain medications. The effective dose in this study was 10 mg per day for 8 weeks (58).
Larger human studies are needed to know if melatonin is safe and effective for endometriosis patients.
Traditional Chinese Medicine
Traditional Chinese medicine (TCM) is used in many parts of the world as a complement to standard medical care.
It incorporates acupuncture, herbal treatments, massage, and other therapies.
Patient testimonials indicate that TCM may provide symptom relief in endometriosis. But scientific evidence is somewhat limited.
Acupuncture
One review of 3 studies found that acupuncture improved pain and quality of life for volunteers. Women in this review received up to 16 treatments either once or twice a week for 15-25 minutes per session (59).
And another study of 67 women with endometriosis found acupuncture to greatly improve menstrual pain (60).
Acupuncture is generally well-tolerated with few side effects and may be worth a try for those dealing with pain.
Herbal Therapies
Herbal preparations have been used for centuries in Chinese medicine to treat various conditions.
One review of 2 small studies found traditional herbal preparations to reduce menstrual pain more effectively than hormonal drugs commonly used in endometriosis. No improvements were seen in rectal, back, or vaginal pain (61).
Herbal therapy isn’t for everyone. Medicinal herbs interact with many medications and are not appropriate for those with certain health conditions.
Summary: The probiotic Lactobacillus and supplemental melatonin are thought to limit endometrial tissue growth. Limited evidence suggests that acupuncture and Chinese herbal preparations may reduce pain. These treatments may be worth trying with a doctor’s approval.
The Punch Line
Endometriosis is largely influenced by hormonal and environmental factors that influence oxidative stress.
Since diet can protect cells against damage, alter hormone levels, and reduce inflammation, a change in eating habits may help lessen symptoms.
Several diet strategies are recommended:
- Eat fewer trans fats and more omega-3 fats. Limit baked goods, processed foods, and fried foods, and aim for 7 ounces (about 200 grams) of fatty fish per week.
- Avoid gluten if you have celiac disease or are sensitive to it.
- A trial of a low FODMAP diet is recommended if you suffer from bowel symptoms.
- Eat at least five servings of vegetables per day, including some leafy green veggies.
- Limit alcohol intake to 1 drink or less per day.
- Ask your doctor if you might benefit from supplemental thiamine, iron, magnesium, or vitamins C, D, E. Probiotics and melatonin have also been reported to reduce endometriosis severity and are recommended with a doctor’s approval only.
- Acupuncture is generally well-tolerated and has been said to reduce pain. It may be worth a try for those with pain during and in between menstrual periods.
Endometriosis is a serious and painful condition, but lifestyle changes and the proper diet can greatly improve health and quality of life.