Traditional treatment of most autoimmune conditions relies entirely on medication.
Graves’ disease has been no exception to that rule.
But recent research indicates eating patterns can and do influence treatment outcomes.
This article looks at the best dietary treatment for Graves’ disease, as shown by current scientific evidence.
What Is Graves’ Disease?
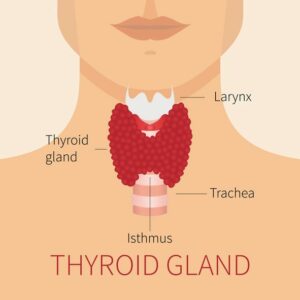
Graves’ disease is an autoimmune disease characterised by an overactive thyroid.
This is known medically as hyperthyroidism, not to be confused with hypothyroidism (such as Hashimoto’s disease).
It was discovered by Dr. Robert Graves in 1835, and has become the most common cause of hyperthyroidism in the developed world (1).
A Graves’ disease patient has a thyroid that produces too much thyroid hormone. It’s caused by unique antibodies called Thyroid Stimulating Immunoglobulins (TSIs), which “mimic” the function of hormones that stimulate thyroid production.
The underlying cause is unknown, but it’s suspected there is a large genetic component at play. Known triggers include infection, stressful life events, high iodine exposure and recent childbirth (2, 3).
Summary: Graves’ disease is an autoimmune disease that overstimulates the thyroid, known as hyperthyroidism.
Symptoms of Graves’ Disease
Graves’ disease symptoms usually occur quickly.
- Weight loss despite increased appetite
- Anxiety or depression
- Irritability and insomnia
- Sweating or heat intolerance
- Irregular heartbeat
- Goitre
- Menstrual irregularity
- Eyesight problems and eyelid swelling
- Mineral imbalances leading to osteoporosis
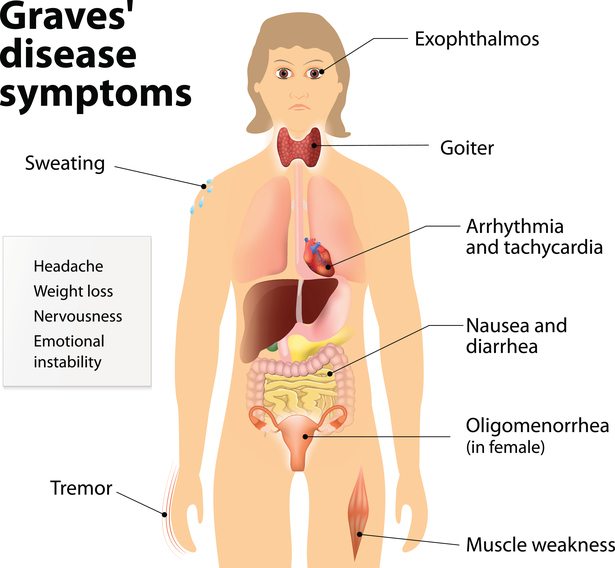
Summary: Common symptoms of Graves’ disease are related to an excessively high metabolic rate.
Medical Treatments for Graves’ Disease
Despite the powerful effects of diet on health, medical treatment is almost always required for thyroid problems.
Graves’ disease is no exception, and there are 3 main treatment options:
Anti-Thyroid Drugs
Anti-thyroid drugs inhibit the body’s ability to create thyroid hormones (5).
The two common types used methimazole (MMI) and propylthiouracil (PTU).
RAI
Radioactive iodine treatment (RAI) is usually the choice after an unsuccessful course of anti-thyroid medication.
It works by damaging or destroying thyroid cells, without irradiating any other cells in the body.
However, 80% of RAI treated individuals end up with hypothyroidism (underactive thyroid) and 10% require additional treatments (6).
Surgery
Surgery is effective, but risky.
It’s usually the last treatment choice and only used on patients who have an extremely enlarged thyroid, or are not suitable for other treatments, such as children.
In fact, surgical removal of the thyroid may be a better choice than RAI for children who fail on anti-thyroid drugs (7).
Summary: Diet is important, but anti-thyroid drugs are the first line of treatment. RAI and surgery are options if the medication is ineffective.
Foods and Nutrients To Eat For Graves’ Disease

Unlike Hashimoto’s disease, diet advice for Graves’ disease is not a common talking point.
Ideally the aim is to develop an eating pattern that helps prevent nutrient-related risk factors of Graves’. The main (somewhat preventable) risk factor is bone mineral loss, best known as osteoporosis (4, 8).
The essential nutrients for optimal bone health include magnesium, calcium and vitamin D.
Magnesium Food Sources
Magnesium is an essential mineral involved in hundreds of bodily processes.
Studies consistently find low magnesium levels are strongly linked with bone mineral imbalances and increased risk of osteoporosis (9, 10, 11).
Considering approximately 68% of US adults do not consume enough magnesium – with 1 in 5 consuming less than half of the recommendations – it should be emphasised more when giving diet advice (12).
The best food sources of magnesium are:
- Leafy green vegetables, like spinach
- Brazil nuts, almonds and cashews
- Pumpkin seeds and sesame seeds
- Fatty fish like mackerel and tuna.
Magnesium supplementation is certainly a great option if you are deficient in magnesium. However, excess magnesium can also be harmful, which is why whole food sources are recommended first (13).
Calcium Food Sources
Calcium is important for bone health, especially as we grow older (14).
The top calcium food sources are:
- Dairy
- Green leafy vegetables, like watercress
- Almonds
- Broccoli.
However, many experts are not sold on the reported benefits of high dairy consumption. And there are numerous ethnic groups with low osteoporosis rates that consume very little dairy, particularly in Asia and Africa (15).
This suggests dietary calcium may not be as important as first thought, which is actually why magnesium is listed first.
Overall moderate dairy intake is safe (and potentially helpful), coupled with regular consumption of leafy vegetables and nuts.
Calcium supplements are also inconsistently linked with beneficial outcomes, but could be a harmless precaution for Graves’ disease patients (16).
As always, speak with your doctor first.
Vitamin D
There is no doubt an increase in vitamin D is beneficial for bone health (14).
The best source is actually regular sunlight exposure. Fatty fish like salmon, tuna and mackerel are good food sources, but far less useful.
In fact, vitamin D is one of the rare exceptions where supplementation is more effective than whole foods sources. Especially in those who are deficient, which is a whopping 42% of Americans (17).
If more time in the sun and more fatty fish is not an option, vitamin D supplementation is strongly recommended after speaking with your doctor. A combination of calcium and vitamin D supplementation is linked to the best outcomes (18).
Summary: Dietary recommendations for Graves’ disease should focus on preventing osteoporosis. That means foods rich in magnesium, calcium and vitamin D. Supplements are also beneficial if the patient has a deficiency.
Foods and Nutrients To Limit

The recommendations here are largely based on medical case-studies and observations.
That means we can form theories or opinions, but nothing should be considered “proven”.
Iodine
Iodine is a mineral required by the thyroid to produce thyroid hormones.
A deficiency in the diet can cause hypothyroidism, and it seems excess can cause or contribute to hyperthyroidism.
There was the case of a woman drinking large amounts of kelp (seaweed) tea each day for 4 weeks under the guidance of a Chinese alternative practitioner. This raised her iodine intake between 3.8 to 6.6 times the recommended daily allowance of 150 μg (19).
She presented to hospital with excessive thyroid hormone levels and multinodular goitre.
Another case-study documented a woman who developed hyperthyroidism shortly after following a high-kelp diet. She had no previous known thyroid issues, which suggests the high iodine intake was a direct cause (20).
Note that iodine-rich food is only an issue when eaten in unusually large quantities, consistently. Kelp, kelp tea, and iodine supplements are the dangers, so you should always speak with your doctor first.
Regular consumption of seafood or sushi should not be an issue.
Gluten
Gluten is a protein found in wheat.
Research shows a link between gluten intolerance (and celiac disease) and antibodies that harm the thyroid. This could have implications for both hypo- and hyperthyroidism.
There have been two documented case-studies of women who were not responding to Graves’ disease medications. In both instances the women were later diagnosed with celiac disease (21, 22).
Interestingly, once going gluten-free they began responding to the Graves’ medications.
Studies actually show that a Graves’ disease patient has an increased risk of celiac disease. In fact, that risk could be up to 4.5 times greater than a healthy person (23, 24).
So there is definitely some sort of connection between autoimmune disease, gluten ingestion and antibodies that harm the thyroid gland.
Screening for celiac disease is fundamental if you have Graves’, and a gluten-free diet could very well be critical.
Soy and Goitrogens
Some speculate that soy and goitrogenic foods can stimulate a potentially harmful immune response on the thyroid.
However this is theoretical, and studies suggest it’s probably not true (25).
Additionally, they’d more likely be a problem for hypothyroidism rather than hyperthyroidism.
As with everything we eat and drink, it’s the dose that makes the poison. It’s very likely that normal amounts are safe. For example, if you eat some tempeh or broccoli at dinner.
That said, unnaturally concentrated sources could theoretically be a problem if you eat them every day in large amounts. Large quantities of soy milk or soy sauce comes to mind.
Summary: Excessive iodine consumption can be harmful, so iodine supplements (including kelp) are not recommended. Gluten may be a problem as the risk of celiac disease is far greater in Graves’ patients. Soy and goitrogenic foods are very likely safe.
Is Graves’ Disease Curable Then?
Graves’ disease is not curable, but very treatable.
About 50% of patients go into remission, with no recurrence of symptoms after that.
This is best achieved with medical treatment and an appropriate, sustainable diet. That includes foods high in magnesium, low in iodine, and maybe even gluten-free.
Other important factors to consider include regular exercise for bone and muscle strength, and reducing chronic stress.