Candida is a fungus that can grow in the human body.
A condition called Candida Overgrowth Syndrome is said to occur if levels in the gut become too high.
But is it actually a real condition, and does diet play a role? This article explores the current research.
What is Candida?

The Candida genus includes more than 20 species of yeast that are able to cause infections in humans (1).
It’s commonly present in the digestive tract and mucous membranes of the nose, throat and reproductive organs.
The most common species is Candida albicans (C. albicans), which is estimated to be present in the mouth or throat of up to 40% of healthy adults (2).
About 70% of healthy adults also have yeasts, mainly Candida species, in their guts (large intestine or bowel) (3).
Summary: Yeasts of the Candida genus are common in the digestive tract and mucous membranes of healthy adults. Some species of Candida can cause infections.
What is Candida Overgrowth Syndrome?
Candida does not cause problems most of the time.
However, sometimes yeasts can multiply rapidly and greatly increase in numbers. This is called yeast overgrowth and can lead to infection.
Yeast overgrowth in the gut can cause a variety of unpleasant symptoms. This has been termed Candida overgrowth syndrome.
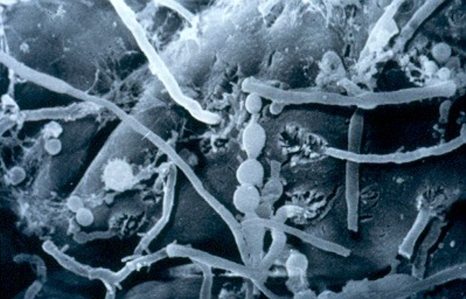
Candida albicans on human small intestine mucosa ( 3000-fold magnification). Click to enlarge (3).
It’s also referred to as:
- Chronic candidiasis
- Candida hypersensitivity
- Candidiasis sensitivity.
While numerous books and diet plans claim to cure the condition, the very existence of Candida overgrowth syndrome is controversial.
It first gained attention in 1984 after the publication of a book by William Crook titled The Yeast Connection: A Medical Breakthrough.
According to Crook, use of antibiotics causes yeast overgrowth (4).
As he explained it, antibiotics kill good bacteria in the gut that usually keep C.albicans in check. With the good bacteria no longer around, Candida is able to multiply and weaken the immune system.
Infections can develop more easily with a weakened immune system. Of course, an infection is typically treated with antibiotics, fueling this cycle.
This theory of Crook’s has never been proven mind you.
Summary: Candida overgrowth syndrome is a controversial condition that some suggest is caused by overgrowth of Candida yeast in the gut.
Other Types of Candida Infection

Some types of Candida infection are well known and described in the medical literature.
Candida infection in the mouth or throat is called thrush. Candida infection of the vagina is commonly referred to as a yeast infection.
More serious infections can occur when Candida enters the bloodstream. This is known as invasive candidiasis. However, most cases occur in hospital or nursing home patients who have weakened immune systems.
There is no scientific evidence that these infections are caused by Candida overgrowth in the gut.
Summary: Infections of the mouth, throat, vagina and bloodstream can be caused by Candida. However, there is no evidence linking these infections with Candida overgrowth in the gut.
Symptoms of Candida Overgrowth

The following symptoms have been attributed to Candida overgrowth syndrome (4, 5):
- Tiredness
- Irritability
- Depression
- Inability to concentrate
- Memory problems
- Hyperactivity
- Headaches
- Rashes
- Constipation
- Abdominal pain
- Diarrhea
- Gas
- Bloating
- Persistent nasal congestion
- Urinary tract problems
- Menstrual irregularities
One issue here is that many illnesses or infections could cause these wide-ranging symptoms. They are not specific to Candida overgrowth.
According to the American Academy of Allergy, Asthma and Immunology, these symptoms are essentially universal. That is, most sick patients probably complain of at least some of them.
Furthermore, there is no scientific evidence to date showing that Candida overgrowth is capable of causing these symptoms.
Summary: Symptoms attributed to Candida overgrowth are not specific and could be caused by a variety of conditions.
Are There Tests to Diagnose It?

Since Candida yeast is present in the majority of people, simply testing for its presence is not useful.
Only one published study has tried to find out whether a set of symptoms or tests could be used to diagnose Candida overgrowth. The researchers could not find any physical or laboratory difference between patients who believed they had Candida overgrowth and those who didn’t (6).
This is in line with what Crook says.
In his book, he suggested yeast may be identified as the cause only when no other conditions are discovered. In other words, yeast would be diagnosed as the cause by ruling out other potential culprits.
Additionally, according to Crook, diagnosis of Candida overgrowth could only be made if the patient responded to a suggested treatment (4).
That is, if symptoms go away following treatment, then Candida must have been the problem.
Summary: There are no laboratory tests or other tests to diagnose Candida overgrowth syndrome.
Is There a Candida Diet?

Many diet books claim to treat or cure Candida overgrowth, including Crook’s.
Some claim they will provide “seemingly miraculous results” and can help you “recover from Candida in 60 days.”
Perhaps the most-well known is the ‘Candida Diet’. Here are the typical recommendations:
- Diet should be nutritionally adequate with fresh foods from a variety of sources.
- Avoid all refined carbohydrates, including sugar, corn syrup, dextrose and fructose.
- Avoid refined, processed and fabricated foods.
- Avoid fruits and milk initially. Later, try to rotate fruits back into the diet if they are tolerated.
- Avoid all yeast and mold-containing foods initially. Ultimately, some of these may prove to be tolerated since a yeast-containing food does not make C. albicans organisms grow.
- Eat sugar-free yogurt.
- Take nutritional supplements, including vitamins, minerals and essential fatty acids.
Unfortunately, there is no evidence that following a so-called ‘Candida diet’ is helpful in treating a candida overgrowth.
Anyone that swaps refined carbohydrates, added sugars and processed foods for whole foods will feel better and experience better health.
It’s no surprise then that patients may feel better following such a diet.
Summary: There is no evidence that a specific candida diet will alleviate symptoms of Candida overgrowth.
Supplements for Candida Overgrowth

The benefit of dietary change is unproven.
But what about the recommendations to take a nutrition supplement?
Keep in mind that Candida is a normal resident of the gut in the majority of healthy adults. Unless a patient has invasive candidiasis, there is no reason to try to reduce Candida.
In fact, according to one group of scientists, eliminating intestinal yeasts is not generally advised (3).
In saying that, many nutrition supplements claim to kill Candida in the gut and/or alleviate symptoms of Candida overgrowth.
However, only probiotics, coconut oil and grapefruit seed extract have some (weak) scientific evidence to back up their claims.
One study found that premature babies given Lactobacillus rhamnosus (a bacterial probiotic) for 12 months were significantly less likely to have Candida in their guts (7). Twenty-three percent of babies given the probiotic had Candida, compared to 48% of those given a placebo.
No published studies have looked at probiotics and Candida overgrowth in adults though.
Then there is coconut oil, which has been shown in lab studies to have antifungal activity (8).
Additionally, one study in mice found those fed a diet extremely rich in coconut oil (50% of total calories) had lower levels of C. albicans in their guts than those fed other types of fat and oil (9).
The authors suggested that coconut oil could potentially be used in humans to reduce C. albicans in the gut, but it remains to be tested.
Summary: Emerging research shows that certain probiotics and coconut oil may be effective in reducing Candida in the gut. However, whether that is beneficial for most peopl is not known.
Antifungal Medicines for Candida Overgrowth

Antifungal medicines have also been suggested as a potential treatment.
One high-quality study looked at the use of Nystatin, an antifungal medicine, in women complaining of Candida overgrowth symptoms. Nystatin was no better than placebo at reducing symptoms (5).
In fact, there’s no published evidence showing that Nystatin or any other antifungal medicines alleviate Candida overgrowth in the gut.
Furthermore, the American Academy of Allergy, Asthma and Immunology states that the long-term use of antifungal medicines is potentially dangerous because it could produce resistant species of C. albicans or other disease-causing fungi (4).
Summary: Antifungal medicines have not been shown to reduce symptoms of Candida overgrowth. In fact, long-term use of these medicines could be dangerous.
Does Candida Cause Leaky Gut Syndrome?

Scientists have shown that C. albicans in the gut can move through the lining of the intestine and into the bloodstream (10).
This is the case in invasive candidiasis.
Because of this, some believe that Candida overgrowth is the cause of increased intestinal permeability, better known as leaky gut syndrome.
However, this is currently an untested theory and we cannot make strong assumptions.
What’s more, leaky gut syndrome presents as a symptom in numerous conditions unrelated to Candida overgrowth.
Summary: There is no evidence that Candida overgrowth causes leaky gut syndrome.
Does Candida Cause Chronic Fatigue Syndrome?

Symptoms associated with Candida overgrowth are similar to those of chronic fatigue syndrome (CFS) and fibromyalgia.
A small study of 20 patients found C. albicans was present in the stool of 60% of CFS patients suffering from severe symptoms (acute phase) compared to only 30% of CFS patients without symptoms (remission) (11).
However, C. albicans was also present in the stool of 53% of healthy control subjects (without CFS) in that study — similar to the acute CFS patients. So it’s unlikely that C. albicans caused CFS in those patients.
Additionally, a controlled trial looking at whether yeast-containing foods affect CFS symptoms found no effect. Patients on a low-sugar, low-yeast diet had no improvements in fatigue or quality of life compared to those on a regular healthy diet (12).
Combined, this evidence suggests it does not cause CFS.
Summary: There is no clear evidence that Candida causes chronic fatigue syndrome. A low-yeast diet also did not improve symptoms in patients with CFS.
Candida and Diet: There Is No Evidence
According to the American Academy of Allergy, Asthma and Immunology, the concept of Candida overgrowth syndrome should be regarded as “speculative and unproven” unless supported by competent research.
And from the current evidence, there is no proof that – if it is a real condition – it is directly responsible for other health issues or disease.
It makes sense then that no specific candida diet or antifungal medicine can help treat it. In fact, no treatment has been shown to consistently eliminate symptoms, which makes me even more skeptical.
If you’ve experienced long-term symptoms associated with Candida overgrowth, talk to your doctor first. There are many potential causes of such symptoms, and more serious issues must be ruled out.
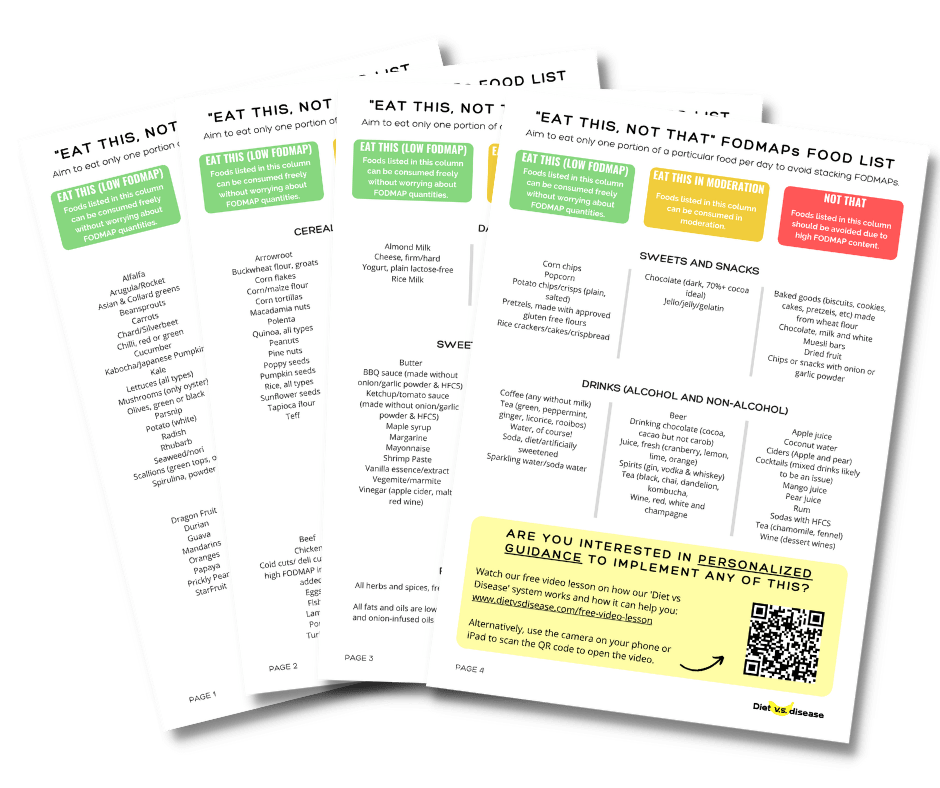
What Can And Can’t I Eat On The Low FODMAP Diet?
Often it’s easiest to start with this giant list I’ve made of what foods to eat, and what foods to avoid when following a low FODMAP diet.
It’s based on the latest published FODMAPs data (1, 2, 3, 4, 5).
Print or save to your phone to use as a quick-reference guide when shopping or cooking. I’ve attempted to list foods in both US and UK/Aus names, with US first.
I’ve included a screenshot of the first page below. But the full PDF is 4 pages and suitable for printing. To download it simply tap the box below and it will then be emailed straight to you – it’s free!