So you’ve had a diverticulitis flare-up.
You’re finally feeling better. But now you’ve got some pain in your joints (maybe some inflammation somewhere in the body) and you’re thinking about taking an anti-inflammatory.
Here’s what a lot of people don’t seem to realize or appreciate (maybe your doctor never told you): Taking NSAIDs—which stands for Nonsteroidal Anti-Inflammatory Drugs—like ibuprofen or Advil, naproxen, or even aspirin increases your risk of another flare-up catastrophically.
We’re talking about a nearly 7 times higher risk of bleeding and a 3 times higher risk of perforation.
It’s like playing Russian roulette with your gut. Every time you take it, you’re dramatically increasing the odds of another flare-up, another ER visit, another round of antibiotics that decimates your microbiome and the resilience of your gut even further.
In this article, I’m going to walk you through exactly what the research shows about NSAIDs and diverticulitis, why they’re dangerous, and what pain relievers you should consider instead.
Of course don’t change anything you do without speaking with your doctor first, but it pays to be well-informed and educated on this.
Here is a video we made, otherwise there is a written version underneath.
The Numbers Don’t Lie
First: The Risk of Getting Diverticulitis in the First Place
A study followed 47,000 men for 22 years and found that people who regularly take NSAIDs have a 72% higher risk of developing diverticulitis (1).
Not only that, the risk of complicated diverticulitis—that means perforation, abscesses, the serious situations that land you in the hospital or needing surgery—more than doubled.
And the longer the use, the higher the risk. After 10 years of regular NSAID use, the risk jumped to an 80% increased risk of diverticulitis.
We’ve spoken with a lot of people who are 60 years and older, and many of them say they used to pop ibuprofen regularly when they were younger, like it was candy, and they believe that contributed greatly to their issues.
Second: The Risk If You Already Have Diverticulitis
This is where the numbers get even more concerning. A meta-analysis looked at 13 previous studies on people who already have diverticulitis. If they take NSAIDs—that’s ibuprofen, naproxen, diclofenac—their risk of diverticular bleeding increases by 7 times. Not double, not triple. Nearly 7 times higher risk (2).
For complicated diverticulitis, the odds ratio was 3.13—suggesting more than triple the risk of serious complications.
The Recurrence Study You Need to Know About
If you’ve already had diverticular bleeding, another study followed patients for a year after their episode (3):
- Among those who stopped taking NSAIDs: only 9% had another bleeding episode.
- Among those who continued taking NSAIDs: 77% had recurrent bleeding.
Stopping NSAIDs reduced the recurrence risk by 94%. Numbers you really can’t ignore.
Summary: Research shows NSAIDs increase initial diverticulitis risk by 72%, with 7 times higher bleeding risk and 3 times higher perforation risk for those with existing disease. Stopping NSAIDs after a bleeding episode reduces recurrence by 94%, from 77% down to just 9%.
Why NSAIDs Can Harm Your Gut
So what’s going on here—why can NSAIDs be so dangerous for your colon, your large intestine?
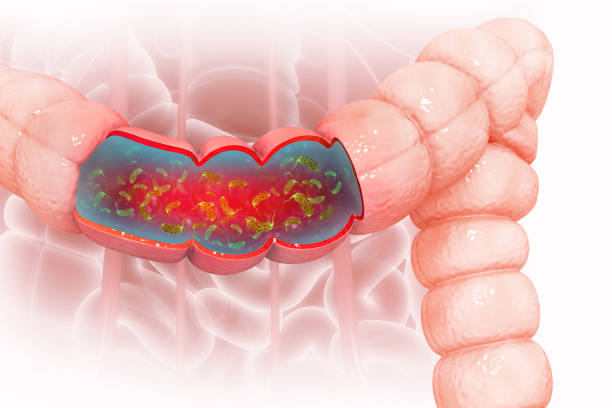
They Break Down Your Gut’s Protective Lining
Think of your intestinal lining like the walls of your house. NSAIDs essentially remove the protective sealant and weather-durable paint that keeps everything watertight.
In the intestine, they thin out the protective mucus layer, making it easier for bad bacteria to get through.
In diverticulitis, you’ve already got these small pouches in your large intestine that are vulnerable spots. When NSAIDs weaken your defenses, bacteria can invade those pouches much more easily. That’s when you get inflammation, infection, and potentially an abscess or perforation.
They Reduce Blood Flow
NSAIDs reduce blood flow to your intestinal lining. Less blood flow means:
- Less oxygen reaching the tissue
- Fewer nutrients are getting to the area
- Reduced ability to heal
Your gut becomes more fragile and more prone to injury—it has less resilience to handle stress or inflammation.
They Prevent Blood Clotting
This is why the bleeding risk is so high—NSAIDs thin your blood. When a small blood vessel breaks in your colon (which can happen in diverticular disease), it can’t seal itself up like it normally would. The bleeding continues and gets worse.
Summary: NSAIDs damage the gut by thinning the protective mucus barrier, reducing blood flow and oxygen to intestinal tissue, and preventing proper blood clotting. This triple threat makes existing diverticular pouches more vulnerable to bacterial invasion, inflammation, and uncontrolled bleeding.
What You Should Take Instead
Option 1: Tylenol (Acetaminophen)
This is the standard recommendation in clinical guidelines, and for most people with diverticulitis, it’s the safest option.
The key is the dose. As I always say, even when we talk about food and nutrition, it’s the dose that makes the poison, right? Guidelines recommend keeping it under 2,000 milligrams per day. Above that, risks start to increase—not just for your gut but also for your liver.

Option 2: Aspirin – It’s Complicated
This is where things get nuanced, because aspirin is an NSAID too, but it works differently from ibuprofen.
The study previously mentioned looked at the effects of aspirin and concluded that regular aspirin use increased diverticulitis risk by 25% and bleeding risk by 70% (4).
That’s lower than non-aspirin NSAIDs like ibuprofen, but it’s still significant.
The Aspirin Dilemma: Heart Health vs. Gut Health
Here’s why this is nuanced: If you’re taking aspirin for secondary prevention (because you’ve already had a heart attack or stroke), most experts agree the cardiovascular benefits outweigh the diverticulitis risks. It makes sense to continue the aspirin.
But if you’re taking aspirin for primary prevention (just for general “heart health” without a history of heart problems), the calculation is different. The bleeding risks may outweigh the benefits, especially if you have diverticular disease.
Important note: You should never change any medication without speaking to your doctor first. I’m not telling you what to do—I’m just a guy on the internet presenting the data and guidelines as we have them. But this is information worth discussing with your healthcare provider.
Summary: Tylenol (acetaminophen) under 2,000mg daily is the safest pain relief option for diverticulitis patients. Aspirin poses lower but still significant risks (25% increased diverticulitis risk, 70% higher bleeding), with the decision to continue depending on whether it’s for primary or secondary heart disease prevention.
If you’re just getting started, download our free Low FODMAP food list to get clarity on common food triggers
Tap the blue button below to download our “Eat This, Not That” list as well as additional resources for Diverticulitis (it’s free!)
What This Means For You
As far as research goes, the findings are profound. Regular NSAID use more than doubles your risk of complicated diverticulitis and increases bleeding risk nearly 7-fold.
So What Should You Do?
Check your medicine cabinet. Make sure you understand what you’re taking. Look for these ingredients:
- Ibuprofen (Advil, Motrin)
- Naproxen (Aleve)
- Diclofenac
- Aspirin (in some cases)
- Any other NSAIDs

Switch to Tylenol for pain relief. Data indicates that keeping it under 2,000mg per day doesn’t increase GI risks. Some sources say you can go higher, but you have to speak to your doctor about your specific situation.
If you’re on aspirin, talk to your doctor. Don’t just stop if it was prescribed for your heart, but have an honest conversation about the risks and whether it’s still the right choice for you, given your diverticular disease.
Consider the long-term impact. If you’ve been taking NSAIDs regularly for years, understand that this may have contributed to your diverticulitis risk and could be making prevention harder.
Summary: Regular NSAID use dramatically increases diverticulitis complications, so checking your medicine cabinet and switching to safer alternatives like Tylenol is critical. Never stop prescribed medications without medical consultation, but have an informed conversation with your doctor about risks versus benefits.
Your Next Steps for Managing Diverticulitis
Understanding the risks of NSAIDs is just one part of successfully managing diverticulitis and preventing future flare-ups. With the right comprehensive approach, you can significantly reduce your risk of recurrence.
What You Need to Know
To truly prevent diverticulitis from returning, you need to address:
- Pain management strategies that don’t harm your gut
- Dietary modifications that support healing
- Lifestyle factors that reduce inflammation
- Warning signs that require immediate attention
Professional Guidance Makes the Difference
If you’re struggling with recurrent diverticulitis or worried about preventing another flare-up, professional guidance can help you navigate all these factors and create a personalized prevention plan.
To learn more, I invite you to apply for a nutrition assessment call with us. We’ll help you make sense of what’s really happening and map out the next steps to get you feeling better—not just temporarily managing symptoms, but addressing the root causes for long-lasting relief.

Leave a Reply