If you’ve been dealing with IBS for a while, you know this feeling all too well. You’re about to leave the house… and suddenly your gut starts churning. You’re at a restaurant, looking at the menu… and the panic sets in. “What if this triggers a flare? What if I can’t find a bathroom? What if I have an accident?”
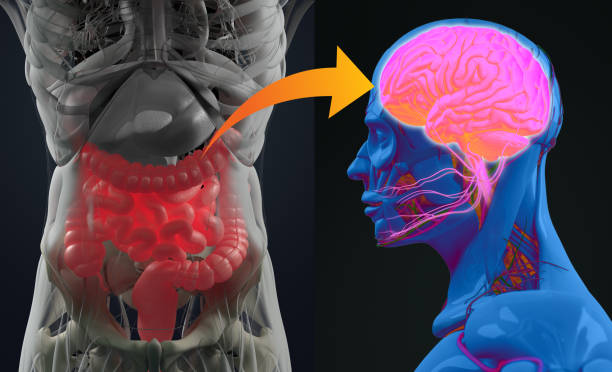
Here’s the thing: this isn’t just in your head. Your anxiety and your gut symptoms are actually connected in a very real, very physical way through something called the gut-brain axis.
When I first started our gut health program back in 2019, I thought it was all about the nutrition. The Low FODMAP diet, identifying food triggers, reducing inflammation — that’s what I focused on. But then something surprising happened. We added a mindset coach to our team, and we started asking clients at the end of the program: “What was the most valuable part for you?” I was expecting them to say the nutrition, the meal plans, and working with the dietitians. However, more than half of them said the mindset work was effective. The anxiety management. Regulating the nervous system.
That’s when I realized: you can’t fix IBS with diet alone.
Here is a video we made, otherwise there is a written version underneath.
Why Anxiety Shows Up With IBS
Before we dive into solutions, let me set the stage here. If you have IBS, there’s a good chance you also deal with anxiety around your symptoms. And it’s not because you’re weak, or overly sensitive, or “making it up.”
It’s because of something called visceral hypersensitivity, which basically means your gut’s alarm system is turned up way too high.
What Is Visceral Hypersensitivity?
Most people don’t feel normal digestion happening. Food moves through, nutrients are absorbed, gas is created, stool is formed, everything just…happens.
But when you have IBS, those normal sensations can feel like alarm bells. A little bit of gas? Feels like a crisis. Some bloating? Panic mode.
Your pain and discomfort are real. They’re physiological. They’re not in your head.
But here’s where it gets tricky: When you’re anxious, you become hyper-aware of every little sensation in your gut. And you feel like you have to act on them. Those sensations trigger more anxiety, which makes you pay even more attention to your gut. And round and round it goes. This is the anxiety-IBS cycle. And it keeps people trapped for years — sometimes decades.
Summary: Visceral hypersensitivity means your gut’s alarm system is overactive, making normal digestive sensations feel alarming and painful. Anxiety amplifies this awareness, creating a self-reinforcing cycle where gut sensations trigger anxiety, which then increases gut sensitivity.
Understanding the IBS-Anxiety Cycle
So now that you understand why anxiety shows up with IBS, let’s talk about what we can actually do about it.
The Gut-Brain Communication Highway
Your gut and brain are in constant communication through what’s called the gut-brain axis. This bidirectional communication happens primarily through the vagus nerve.
IBS involves visceral hypersensitivity, which includes:
- Visceral hyperalgesia – an exaggerated pain response to stimuli
- Allodynia – when sensations that aren’t normally painful start to become painful
What this means practically is that normal digestion processes that most people wouldn’t notice can trigger significant discomfort if you have IBS.
Why This Isn’t Your Fault
Your pain is real, and it is physiological. It’s not something you’re imagining. This isn’t caused by anxiety, but here’s what happens: When we’re anxious, we become more tuned into gut sensations. We become more hyper-aware. And those sensations themselves can then trigger more anxiety.
Your gut sends signals up to the brain, and your brain sends signals back down to your gut in this two-way street. This isn’t your fault. It’s not a personal failing. It’s how the nervous system has learned to respond.
Summary: The gut-brain axis creates bidirectional communication where gut sensations trigger brain responses and vice versa. IBS involves heightened pain sensitivity that makes normal digestion feel alarming, and anxiety amplifies this awareness, but this learned response pattern is not a personal failing.
The Role of Trauma and Genetics
A lot of people blame themselves for feeling anxious about their gut. So how much of this is actually within their control, and how much of it is just biology doing its thing?
The Genetic Component
There is generally some genetic predisposition to gut issues. When working with clients, we often ask: Did your parents or siblings have digestive issues? If we don’t see gut issues in the family, we often see them on the mental health side instead.
We’re all predisposed to something when we come into this world, and then it’s our own lived experience that can express it.
Understanding Trauma
When most people think of trauma, they think of PTSD or something major. But trauma is actually subjective — no one can tell you what was traumatic in your history or not.
Trauma can be:
- Small “t” traumas that accumulate over time
- Big “T” traumas like major life events
- Cumulative stress and dysregulation
- Medical dismissal and feeling unheard
- Living with symptoms for years without answers
Some of the newest research shows that cumulative little “t” traumas can sometimes be more detrimental than those bigger “T” traumas.
How This Affects IBS
For many people with IBS, there’s often:
- A genetic predisposition (family history of gut or mental health issues)
- Some level of trauma or chronic stress
- Medical dismissal or rejection from healthcare providers
- Shame and embarrassment prevent seeking help early
When you don’t feel safe, when you don’t feel heard, when you don’t know what’s causing your symptoms, you feel hopeless and helpless. This dysregulation of the nervous system can exacerbate IBS symptoms.
Summary: IBS often has genetic components running in families, either as digestive issues or mental health conditions. Trauma (both big and small) and chronic stress can dysregulate the nervous system and trigger symptom expression, while medical dismissal compounds feelings of helplessness and anxiety.
If you’re just getting started, download our free Low FODMAP food list to get clarity on common IBS triggers
Tap the blue button below to download our “Eat This, Not That” list as well as additional resources for bloating (it’s free!)
Step 1: Retraining Your Nervous System
Here’s the good news: your nervous system learned to respond this way, which means it can also learn a new way to respond.
Nervous System Regulation: Your Daily Practice
The first step is teaching your body safety again through nervous system regulation. The research shows that daily calming practices, even for 10 to 20 minutes, keep the nervous system more balanced overall.
The Strongest Evidence: Gut-Directed Hypnotherapy
Gut-directed hypnotherapy specifically has the strongest evidence for IBS symptom relief or reduction. But there are other evidence-based options as well:
Effective Nervous System Regulation Techniques:
- Gut-directed hypnotherapy (Level A evidence)
- Diaphragmatic breathing (4-7-8 technique or breathing into a straw)
- Progressive muscle relaxation (tensing and releasing muscle groups)
- Yoga Nidra (body scan meditation)
- Various breathing techniques (mountain breathing, square breathing)

The Toothbrush Analogy
Think of nervous system regulation like brushing your teeth. You don’t just do it when there’s a problem. You do it daily to prevent something from happening.
When establishing the practice:
- Try to do it daily rather than waiting for a crisis
- If going through something heightened, try twice daily (morning and night)
- Even 30 seconds of breathwork between activities can help
Understanding Diaphragmatic Breathing
Your diaphragm is a muscle underneath your lungs, but above your stomach and gut. When you breathe in, it should expand like a balloon (your belly gets bigger), and when you breathe out, it should contract (your belly pulls in).
How to practice:
- Raise your arms overhead (optional but helpful for learning)
- Breathe in through your nose – your stomach should expand outward
- Breathe out through your mouth – your stomach should contract inward
- The hand on your belly should move more than the hand on your chest
This type of breathing directly impacts vagus nerve sensitivity and helps shift you into “rest and digest” mode.
Building the Habit
If you’re struggling to implement the habit, stack it onto something you already do:
- After brushing your teeth, do 5 rounds of breathing
- Before bed, listen to a guided meditation
- Between work tasks, shake out your body and do 30 seconds of breathwork
Attach it to something automatic, and it becomes easier to maintain.
How Long Does It Take?
When you do a full nervous system education and practice consistently, you generally start to see what’s called a bioplasticity reset around six weeks.
Just as the brain is capable of neuroplasticity (great change), your nervous system is capable of bioplasticity. As you start to understand what your body is doing and work with yourself during the day through somatic activities and breathwork, you start to see a widening of your window of tolerance.
In six weeks, something that would have been a big deal becomes manageable. You handle things better. You notice you didn’t have anxiety before that medical appointment, or something happened, and you didn’t give it a second thought.
Summary: Daily nervous system regulation practices (10-20 minutes) can retrain your body’s stress response, with gut-directed hypnotherapy showing the strongest evidence for IBS relief. Consistency is key, and within six weeks of regular practice, you’ll start seeing a “bioplasticity reset” where your window of tolerance widens and previously triggering situations become more manageable.
Step 2: Changing the Story You Tell Yourself
Regulating your nervous system is step one in overcoming IBS anxiety. But there’s another piece to this puzzle — and it’s just as important. You need to start transitioning away from fear-based thinking and the negative story you’re telling yourself about your gut symptoms.
Understanding Fear-Based Thinking Patterns

The fear-based thinking in IBS has really specific patterns. It sounds like:
- “What if this meal ruins my day?”
- “I don’t think this is low FODMAP…”
- “This pain means something is seriously wrong with me.”
These thoughts are powerful triggers for your nervous system.
Cognitive Behavioral Therapy Techniques
We use cognitive behavioral therapy (CBT) techniques, specifically adapted for IBS:
Reframing means shifting from “this is dangerous” to “this is uncomfortable, but it’s not dangerous.” Cognitive diffusion is one of the most powerful skills we teach. It’s part of Acceptance and Commitment Therapy (ACT), and it helps you see that your thoughts are just thoughts. They’re not facts.
How to Practice Cognitive Diffusion
Instead of embodying your negative thoughts immediately, we want you to step away and examine them first.
The process:
- Notice you’re having a negative thought
- Ask yourself: “What am I believing to be true?” or “What’s the story I’m telling myself?”
- Separate yourself from the thought – put it in front of you instead of letting it be a cloud above your head
- Say to yourself: “I notice I’m having that thought” instead of “I am anxious”
Examples of Cognitive Diffusion
One technique is to name your anxiety or catastrophic thinking:
- “Oh, amazing! Catastrophe has come to visit my brain. What are we believing to be true today?”
- “Not today, Brian. We are not doing that today.”
- Some people even sing the fear out loud – when it sounds ridiculous, you can laugh, and when you’re laughing, you’re not believing the thought
The Importance of Language
There’s a huge difference between:
- “I am my anxiety” vs. “I notice I’m having an anxious thought”
- “I am my IBS” vs. “I have IBS symptoms right now”
You are not your IBS. You are not your anxiety. These are experiences you’re having, not your identity.
Anchoring Rituals Before Eating
We pair cognitive techniques with anchoring rituals – small calming practices before eating that start to signal safety to your nervous system:
- Do diaphragmatic breathing before meals
- Light a candle and make mealtime special again
- Eat in a different place if your usual spot has bad associations
- Practice gratitude for everything that brought the meal to your table
- Don’t rush your food
When your system is relaxed before you start eating, it aids digestion significantly.
Summary: Fear-based thinking patterns like “this is dangerous” or “something’s seriously wrong” trigger nervous system responses that worsen symptoms. Cognitive diffusion techniques help you recognize thoughts as just thoughts, not facts, while anchoring rituals before meals signal safety to your body and improve digestion.
Step 3: Building Safety Around Food
One of the biggest sources of anxiety for people with IBS is food. You’re scared to eat. You’re scared to try new things. You’re scared of triggering a flare.
And I get it. Food is one of the most common triggers. But here’s what happens when that fear takes over: You start restricting more and more foods — not because they actually trigger symptoms, but because you’re afraid they might. And that fear starts to outweigh the actual risk.
The Problem With Food Restriction
Food anxiety is one of the biggest challenges we see with IBS. While some foods may genuinely trigger symptoms, food fear often exceeds the actual risk.
The principle: What we resist persists.
If you have a fear of dogs and never go near them, that fear grows bigger and bigger. It’s the same with food. If you continue to resist certain foods, the fear starts to outweigh the actual risk.
What happens is people start restricting more and more foods based on fear rather than actual evidence, and that worsens both anxiety and nutritional status.
Why Working With a Trained Dietitian Matters

A lot of clients have gone to a GI doctor and been handed one sheet of paper saying, “Here’s a low FODMAP diet, off you go.” This is a therapeutic diet. You need your hand held through it.
This is why working with an IBS-trained dietitian is crucial – someone who:
- Uses graded exposure techniques
- Knows the FODMAP protocols and nuances
- Can identify if it might be histamine, SIBO, or something else
- Knows how to reintroduce foods systematically
The Graded Exposure Approach
When reintroducing foods, dietitians use graded exposure:
- Start with foods that are generally well-tolerated
- Begin with small doses (so if you have a reaction, it’s a small one)
- Practice calming techniques while eating
- Gather evidence that challenges the fear story
The goal: You’re going through a little period of unpredictability for a future of predictability, as opposed to constant unpredictability.
The IBS First Aid Kit
Yes, we encourage having an IBS or anxiety first aid kit for emergencies. But we’re not just preparing for disaster – we’re actively teaching your nervous system that eating can be safe and showing you the roadmap to do that with both food and mindset in mind.
Summary: Food fear often exceeds actual risk, leading to unnecessary restriction that worsens both anxiety and nutrition. Working with an IBS-trained dietitian who uses graded exposure techniques helps you systematically reintroduce foods while practicing calming techniques, gathering evidence that eating can be safe.
Step 4: Self-Compassion and Connection
The last step is self-compassion. I know that might sound fluffy or “woo-woo,” but it’s scientific and evidence-based. Most people with IBS are incredibly hard on themselves. They feel ashamed of their symptoms. They feel like a burden. They blame themselves for not “getting better fast enough.”
But here’s the truth: Having gut issues is not a character flaw. It’s not a choice. And you deserve kindness — especially from yourself.
Why Self-Compassion Matters
IBS can make people feel really alone, isolated, and ashamed. Bathroom symptoms, food restrictions, the unpredictability – they can trigger deep shame and guilt.
But here’s what research shows: Self-compassion isn’t just being nice to yourself. It actually reduces IBS symptom severity and improves quality of life.
The Three Components of Self-Compassion
According to Dr. Kristin Neff, self-compassion has three parts:
- Self-kindness instead of harsh self-criticism – We’re going to move to change quicker when we’re loving ourselves through it than if we’re being awful to ourselves
- Common humanity – Recognizing that suffering is part of being human rather than feeling isolated
- Mindfulness – Being mindful of your pain without getting completely overwhelmed by it
Practical Self-Compassion Strategies
What this looks like in practice:
- Talk to yourself like you would a good friend
- Reach out for connection (social connection is so important)
- Engage in activities that bring meaning or joy
- Actively challenge shame by reminding yourself this is a medical condition affecting millions – it’s not a character flaw or choice
- Write positive affirmations on your bathroom mirror
Why Self-Judgment Is So Damaging

When you’re being critical of yourself, it’s like someone externally being critical of you – but probably worse, because you’re actually believing it when you say it to yourself.
Your body responds to negative self-talk:
- You feel heavy
- Your posture collapses
- Signals go up the vagus nerve and back down
- Your body enters a helpless, hopeless, depressive state
This dysregulation affects your immune system, hormone function, and even your inflammatory markers.
However, when you offer kindness to yourself and regulate your nervous system:
- You’ll start to see improvements in your immune system
- You’ll start to see improvements in inflammatory markers
- You’ll extend more kindness to other people
- Your inner world becomes a reflection of how you treat others
The more self-compassion you offer yourself, the more kindness you extend to other people.
Building the Self-Compassion Muscle
For some people, self-compassion can be really hard at first. Talking kindly to yourself might feel strange. But it’s like a muscle – if you struggle with meditation, chances are you’ll also struggle with self-compassion if you’ve had a strong inner critic for a long time.
Start small and notice whose voice that inner critic is using (a parent, sibling, teacher?), challenge it actively, practice daily, even when it feels awkward. And lastly, don’t forget to celebrate small wins!
At the end of the day, you should be able to say: “You aced that, babe. Well done.”
Summary: Self-compassion (self-kindness, common humanity, and mindfulness) is scientifically proven to reduce IBS symptom severity and improve quality of life. Harsh self-criticism triggers nervous system dysregulation that affects immunity, hormones, and inflammation, while self-kindness promotes healing and extends to how you treat others.
Your Next Steps for Healing IBS Anxiety
If you’re sitting here thinking, “Okay, this makes sense. But how do I actually implement all of this?” — That’s exactly what we help people with inside our program.
You get a dietitian who walks you through the food side step-by-step, and a mindset coach who teaches you these nervous system regulation techniques and helps you break those thought patterns. It’s not just information — it’s implementation.
To learn more, I invite you to apply for a nutrition assessment call with us. We’ll help you create a personalized plan that addresses both your gut and your anxiety — not just temporarily managing symptoms, but addressing the root causes for lasting relief.

This article was absolutely excellent. I have anxiety have had it for a long time and also have had IBS for a long time. I never thought the two were related, but after reading your article I understand and it makes sense. I am going to try the breathing exercises that you recommended. I’m not young. I’m in my 80s and I have had this for many years. The anxiety and stress have been with me also for many years. I think I am going to try and find some peace for whatever years I have left. Thank you so much.
Another way to check diaphragmatic breathing is to lay down flat on the bed or floor, placing the palms of the hand on the diaphragm gently, relaxing and breathing gently then deeply. Try not to raise your shoulders but focus on the diaphragm. This is what I was taught when studying voice and has served me well into my late 80s.
Unbelievably comprehensive. There isn’t a question left after reading this detailed version of life with IBS. It’s like nothing I have read before and everything I needed to understand and move forward equipped, now, to face every former dilemma With a roadmap now my FodMap!
Thank you! What a gift!
L. D. Sanders