If you’ve ever had IBS symptoms that come with bladder urgency, pelvic pain, or just feel like your whole lower body is out of sync…
You’re not imagining it.
The gut, the brain, and the bladder — plus the pelvic floor — are all part of the same network. And if you don’t understand how they influence each other, you’ll never get full relief.
This is a monumental missing link in gut health that I want to unpack for you today, and it’s especially important if your approach has always been limited to diet changes and hasn’t really helped your gut.
In this article, I’m going to give you a quick foundation so you understand what the gut-brain-bladder axis is, why it matters, and how to restore balance when this axis becomes disrupted.
Here is a video we made, otherwise there is a written version underneath.
The Importance of the Gut-Brain-Bladder Axis
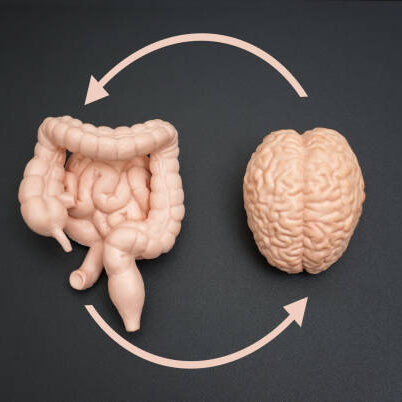
The gut-brain-bladder axis is the communication highway between your digestive system, your urinary system, and your nervous system — all connected by neural pathways and chemical messengers.
At the center of this is the vagus nerve — the longest cranial nerve in the body. It runs from your brainstem down to your gut, bladder, and reproductive organs. It helps regulate digestion, inflammation, mood, and even your immune system.
But here’s the issue…
When you’re under chronic stress or anxiety, your body flips into “fight-or-flight” mode, activating the nervous system.
That fight or flight response is helpful in short bursts, like if you need to run from danger. But when this stress mode is always on, it causes muscles throughout the body to tense up, especially in the pelvic floor.
If the pelvic floor is tense from chronic stress or anxiety, it affects everything — digestion, elimination, even how your bladder and bowels feel day to day. That’s why it’s important to start focusing on the process of moving you out of ‘fight or flight’ and into what we call ‘rest and digest’ mode.
Summary: Your gut, bladder, and brain are all part of the same communication network. Chronic stress or anxiety creates tension that disrupts this network — making IBS symptoms harder to resolve.
Step 1: Understand Pelvic Floor Dysfunction and Nervous System Dysregulation

Now that you’ve seen how tension in the pelvic floor can disrupt both your gut and bladder, we need to get more specific, because not all pelvic floor issues look the same.
Some people have muscles that are too tight, leading to cramps, urgency, or constipation.
Others have muscles that are too weak or uncoordinated, which can cause leaking, incomplete emptying, or even prolapse.
And then there are folks stuck in the middle, with muscles that fire at the wrong time altogether.
When the pelvic floor isn’t functioning properly — whether it’s too tight, too weak, or simply out of sync — it throws everything off.
Think of your pelvic floor as the shock absorber in a car. It cushions and regulates movement — but when it’s too stiff or too loose, every bump feels exaggerated. That tension sends false alarms to your brain — like urgency or pain — when nothing’s actually wrong.
That’s why we always say: if your gut symptoms haven’t improved with diet alone… your pelvic floor might be the missing piece.
How To Identify and Support Pelvic Floor Dysfunction
You may need to work with a pelvic floor therapist or gut-directed therapist to help identify what’s really going on. But in the meantime, know this:
- Chronic stress and trauma (even subtle or long-term) can create protective tension
- That tension leads to poor coordination between the gut and the bladder
- This creates false signals of urgency, pain, or discomfort
Summary: If your IBS symptoms include bladder issues, urgency, or pain, you may have pelvic floor dysfunction driven by nervous system dysregulation. Supporting your nervous system and relaxing your pelvic floor is essential.
If you’re just getting started, download our free Low FODMAP food list to get clarity on common gut triggers
Tap the blue button below to download our “Eat This, Not That” list as well as additional resources for IBS (it’s free!)
Step 2: Healing Requires Safety — Not Just Willpower
Let’s talk about something most gut programs never address: Trauma.
Not just the big kind, but the chronic, low-level kind:
- Toxic work environments
- Family stress
- People-pleasing habits
- Medical anxiety or bathroom fear
When your nervous system is always braced for danger, your gut and bladder cannot relax. This shows up as:
- Inflammation
- IBS symptoms
- IC symptoms
- Hormonal imbalances
And this matters because your brain isn’t wired to make you happy. It’s wired to keep you safe.
So if you’ve had bad experiences — urgency, accidents, embarrassing moments — your brain starts ringing alarm bells automatically. Even when there’s no real threat.
This creates a loop that keeps you stuck.
How To Break The Cycle
We teach our clients how to gradually retrain their nervous system using:
- Breathwork
- Body awareness
- Grounding exercises
- Trauma-informed support
- And yes, tools like a Squatty Potty to support relaxed elimination
That last one might seem silly, but it’s one of the most practical changes you can make. Humans evolved to squat — not sit — and when you raise your knees, it helps relax the pelvic floor and straighten the rectum.
Summary: Lasting gut relief requires a nervous system that feels safe. Trauma, stress, or fear create bracing patterns that diet alone can’t solve.

What About Food?
If you’ve done food eliminations and they didn’t help long-term…now you know why. We still use food protocols — like the Low FODMAP diet — to identify triggers. But we combine it with:
- Nervous system support
- Pelvic floor awareness
- Gut-brain therapy
That’s the difference between symptom control and real healing.
Summary: Food is one piece of the puzzle. Without nervous system and pelvic support, the gut can’t heal fully even with the perfect diet.
What Should You Do Next?
If you’ve tried it all and nothing sticks, please know you’re not broken and there is a solution.
Your body is just stuck in a pattern that it never got the chance to unlearn. But it can unlearn. And when it does? The results speak for themselves: a gut that finally feels predictable again, less urgency, less pain, and more confidence.
If you suspect your gut issues are tied to your nervous system or pelvic floor, we can help you. To learn more, I invite you to apply for a nutrition assessment call with us.
The gut-brain-bladder axis and related digestive disorders are what we specialize in, and we are the world’s leading team to do this online.

This is interesting , being that i have gone through 44 years of IBS, ( C) a 6 week period of extreme (D) finally diagnosed using colonoscopy & biopsy to have microscopic colitis, now reversed again , but under control using natural remedies , & SSRIs ( for extreme anxiety) . Only recently has urgency hit my bladder often brought on by running water, tap, garden hose, pond airpump etc! At 84 yo I just thought it was because i was reaching old age!