Every year, diverticulitis is responsible for over 300,000 hospital admissions in the US alone. And that rate is increasing every year.
Here’s what’s really concerning — most patients have never even heard of diverticulitis until they’re in the emergency room. But there are 7 specific warning signs that could help you catch this condition early, before it becomes a medical emergency.
Some of these signs are so subtle that even doctors miss them. Others show up in completely different parts of your body that you’d never connect to your digestive system. Understanding these warning signs could mean the difference between catching diverticulitis early and ending up in the ER.
Here is a video we made, otherwise there is a written version underneath.
Warning Sign #1: Pain in the Lower Left Quadrant
The first warning sign isn’t just pain — it’s WHERE the pain shows up, and this is where most people get confused.
Diverticulitis occurs when small pouches (called diverticula) that develop in weakened areas of your colon wall become inflamed or infected. These pouches predominantly appear in the sigmoid colon, located in your lower left abdomen.
Your abdomen can be divided into four quadrants using your belly button as the center point:
- Right Upper Quadrant (RUQ): Where your liver and gallbladder sit. Pain here often points to gallbladder disease or liver problems.
- Left Upper Quadrant (LUQ): This quadrant holds your stomach and spleen. Pain here can be mistaken for ulcers or pancreatitis.
- Right Lower Quadrant (RLQ): Where your appendix is located, so pain here raises concern for appendicitis.
- Left Lower Quadrant (LLQ): Where your sigmoid colon lives — and where diverticulitis usually strikes.
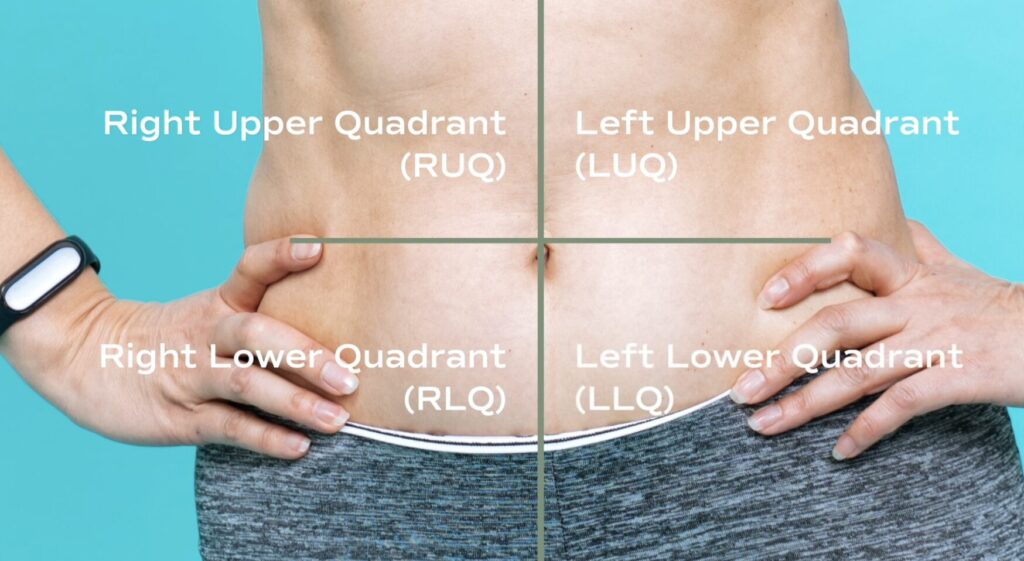
In most people, diverticulitis pain is steady, sharp, and localized to the left lower side of the abdomen. However, research shows that in Asian populations, diverticulitis can occur in the right lower quadrant instead, making it easy to confuse with appendicitis.
The key pattern to watch for is pain that starts vague, then becomes localized and constant. Unlike other types of abdominal pain that come and go, diverticulitis pain tends to stay put and gradually intensify.
Summary: Diverticulitis typically causes steady, localized pain in the lower left abdomen that progressively worsens, though location can vary by population. The pain pattern is distinct from other abdominal issues because it remains constant rather than coming and going.
Warning Sign #2: Fever and Night Sweats That Most People Ignore
Here’s what you need to understand about diverticulitis — it’s an infection, and when your body fights an infection, you typically develop a fever. That’s your immune system responding to the infection in your colon.
What’s really telling is the pattern many patients describe. One person shared: “I get night sweats so bad I sleep on towels. My lower left abdomen gets hot.” This localized heat, combined with night sweats, is your body’s inflammatory response to the infection.
Now here’s what’s surprising — research shows that about 15% of diverticulitis patients are completely afebrile, meaning they have no fever at all or only high-range normal temperatures. Many patients dismiss their low-grade fevers, thinking they’re just run down or fighting off a cold.
Just because you don’t have a fever doesn’t mean you should dismiss other symptoms. But when you do have a fever, especially combined with abdominal pain, that’s a significant warning sign that warrants same-day medical evaluation.
Summary: Fever and night sweats are common inflammatory responses to diverticulitis infections, though 15% of patients never develop fever. The combination of fever with abdominal pain requires immediate medical attention, but lack of fever shouldn’t lead to dismissing other warning signs.
Warning Sign #3: Bowel Changes That Seem Mixed
Diarrhea and constipation can both be symptoms of diverticulitis, but patients often describe specific patterns that doctors frequently miss.

One patient described their progression: “It starts as a pain in the lower left abdomen… Then the bowel movements start to change quickly. Less and less frequent.” They then described taking multiple trips to the toilet in the morning to pass stools that came out like “rabbit pellets.”
Another patient shared: “It’s bloating, cramps, and little diarrhea alternating with brief constipation. Just all-around misery, happens out of nowhere.”
The key is recognizing when these changes differ from your normal pattern, especially when they’re sudden changes accompanied by abdominal pain. These aren’t the gradual shifts you might experience with dietary changes — they’re abrupt alterations that seem to happen without explanation.
Summary: Diverticulitis causes distinct bowel pattern changes including alternating diarrhea and constipation, reduced frequency, or small pellet-like stools. The critical factor is sudden changes from your normal pattern, especially when paired with abdominal pain.
Want more gut-friendly foods that won’t trigger symptoms? Download our free Low FODMAP food list
Tap the blue button below to download our “Eat This, Not That” list as well as additional resources for bloating (it’s free!)
Warning Sign #4: Urinary Symptoms That Fool Everyone (Including Doctors)
This might surprise you, but diverticulitis can cause urinary symptoms that are often mistaken for a urinary tract infection.
Here’s why: your sigmoid colon sits very close to your bladder. When diverticular pouches become inflamed and swollen, they can push against the bladder and cause symptoms like painful urination, frequency, and urgency.
In more serious cases, something called a fistula can form — an abnormal connection between the colon and bladder. One patient shared: “I had none of the usual symptoms until the fistula had broken out and made my bowel join with my bladder. My first sign was air bubbles when I was urinating and I experienced a burning feeling.”
The Danger Signs to Watch For:
- Pneumaturia: Air bubbles in your urine
- Fecaluria: Feces appearing in your urine
- Recurrent “UTIs”: Especially in someone with known diverticular disease
The key point is that if you have urinary symptoms combined with abdominal pain, don’t assume it’s just a UTI — especially if you’ve had digestive issues before.
Summary: Diverticulitis can cause urinary symptoms due to the colon’s proximity to the bladder, often leading to misdiagnosis as UTI. Warning signs include air bubbles in urine, recurrent infections, or painful urination combined with abdominal pain.
Warning Sign #5: Pain in Unexpected Places

This might sound strange, but diverticulitis can cause pain in places that seem to have nothing to do with your gut.
One patient described their experience: “I get what feels like pain in my groin, hip, or my upper thigh. As a teen, I used to get this when I had bad menstrual cramps.” That comparison to menstrual pain is actually quite telling — both involve inflammation that can affect the same nerve pathways.
But it gets even more unusual. Another patient shared: “In a flare-up up my symptoms are cold hands and generally a panicky feeling with a tight chest. Also, my left leg feels numb (same side as the diverticulitis).”
How Can a Colon Problem Cause These Symptoms?
When you have significant inflammation in your body, it triggers a systemic response. Your nervous system can interpret and refer this inflammation to other areas, sometimes mimicking anxiety symptoms or even heart problems.
This is why diverticulitis often gets mistaken for completely different conditions. Patients have reported being misdiagnosed with:
- Kidney stones
- Ovarian cysts
- Endometriosis
- “Just menstrual cramps”
When you have multiple unexplained symptoms happening together — abdominal pain plus unusual sensations in other parts of your body — it might all be connected to the same inflammatory process in your gut.
Summary: Diverticulitis inflammation can cause referred pain in unexpected locations including groin, hips, thighs, and even chest tightness or leg numbness. This systemic inflammatory response often leads to misdiagnosis of unrelated conditions like kidney stones or gynecological issues.
Warning Sign #6: Atypical Presentations in Different Age Groups
Diverticulitis doesn’t always present the same way across different age groups, which is why it’s so often missed.
In Older Adults (65+)
Research shows that diverticulitis in elderly patients often presents with systemic symptoms without obvious localized pain. Instead of the classic left-side pain, older adults might present with:

- Fatigue
- Fainting episodes
- Acute kidney problems
A 2025 study concluded: “CT imaging should be considered in any patient over 65 suspected of having diverticulitis and presenting with systemic signs or atypical symptoms such as fatigue, syncope, and/or acute kidney injury” (1).
In Younger Patients (Under 50)
About half of diverticulitis cases now occur in people under age 50, as it’s becoming increasingly common. However, these younger patients often face skepticism from healthcare providers.
The concerning part? Young patients are twice as likely to be misdiagnosed, yet they often have more aggressive disease requiring surgical intervention more frequently than older patients.
The Cases That Don’t Hurt Much
Perhaps most dangerous are the cases that don’t cause severe pain. One patient said: “The two times I had confirmed diverticulitis (with CT scan) I never had what I would consider lots of pain. I felt uncomfortable, like in my gut, but that’s it.”
This illustrates that some cases present as dull, persistent discomfort rather than severe pain, which can delay people from seeking care.
Summary: Diverticulitis symptoms vary significantly by age, with elderly patients showing systemic symptoms like fatigue instead of typical pain, while younger patients face higher misdiagnosis rates despite more aggressive disease. Some cases present with only mild discomfort, making them particularly dangerous due to delayed treatment.
Warning Sign #7: Persistent Bloating and Gas That Won’t Resolve
This warning sign is one that many people dismiss, but it shouldn’t be overlooked — especially when it occurs alongside other symptoms we’ve discussed.
Persistent bloating and trapped gas are actually quite common in diverticulitis, but they’re often written off as “just IBS” or normal digestive issues, which delays proper diagnosis and treatment.
What Makes This Different from Regular Bloating?
With diverticulitis, patients often describe feeling like they can’t pass gas at all. This inability to pass gas during flares is actually quite common and ties in with the bloating and partial blockage that can occur.
The bloating also tends to be more severe and localized. Many patients report that their lower abdomen feels distended and tender to the touch, not just generally bloated like you might feel after a large meal.
The Key Distinction
Bloating and gas issues are symptoms of many digestive conditions, including IBS. But when bloating is:
- Persistent and doesn’t respond to usual remedies
- Combined with other warning signs like left-side pain
- Accompanied by low-grade fever or changes in bowel habits
That’s when it becomes more concerning and warrants medical evaluation.
Summary: Persistent bloating and inability to pass gas are common diverticulitis symptoms often dismissed as IBS. The key distinction is localized, severe bloating that doesn’t respond to typical remedies and occurs with other warning signs like pain or fever.
When to Seek Medical Attention
The point of understanding these warning signs is to know when something doesn’t add up and you need a thorough workup with your doctor.

Don’t Accept “It’s Probably Just IBS” If You Have:
- Multiple warning signs occurring together
- Sudden changes in your typical symptom pattern
- Symptoms that don’t respond to usual treatments
- Any combination of abdominal pain with fever
For those who’ve already been diagnosed, learning to recognize these symptoms can be transformative on your journey with this condition. While the symptoms can be frightening, understanding what’s happening in your body empowers you to take appropriate action at the right time.
Summary: Seek immediate medical attention if you have multiple warning signs together, especially fever with abdominal pain, or if symptoms don’t match typical IBS patterns and fail to respond to standard treatments.
What Should You Do Next?
If you’re worried about diverticulitis returning, or you don’t feel confident in managing it, you don’t have to navigate this alone. We’ve helped thousands of people get real clarity on what’s happening with their gut and create a personalized plan to address it.
Understanding these seven warning signs empowers you to:
- Recognize symptoms early before they become emergencies
- Avoid misdiagnosis and get proper treatment faster
- Communicate more effectively with your healthcare providers
- Take appropriate action when symptoms arise
With the right comprehensive approach, you’ll know exactly what to watch for and when to seek help.
To learn more, I invite you to apply for a nutrition assessment call with us. We’ll help you make sense of what’s really happening beneath the surface and map out the next steps to get you feeling better — not just temporarily managing symptoms, but addressing the root causes for long-lasting relief.

Hi Everyday as soon as I wake up before taken my diabetic and iron pills , as soon as I wake up I fell like vomiting 🤢, is that has to do with my diverticulitis disease?? Plus today is started today after my iv infusion appointment I can’t poop